January 5, 2009 — In a study to determine the diagnostic value of molecular imaging in nodal staging of patients with thyroid cancer, researchers were able to accurately distinguish between cancerous cells in regional lymph nodes and normal residual thyroid tissue directly after surgery for the first time.
Researchers from the University of Erlangen-Nürnberg, Germany, reported in an article in the January issue of The Journal of Nuclear Medicine on the results of a study using a hybrid single photon emission computed tomography-computed tomography (SPECT-CT) camera to determine and locate the spread of cancer cells to nearby lymph nodes.
According to the researchers, the demonstration or exclusion of cancer spread (metastasis) in regional lymph nodes plays a major role in treating the disease since all patients with lymph node metastases are considered to be at high risk for recurrence.
Currently, patients with differentiated thyroid carcinoma (DTC) who have had their thyroid removed are treated with radioactive iodine, which effectively zeros in on and kills any remaining cancerous thyroid cells. Because one of the functions of the thyroid gland is to absorb iodine from the blood, radioiodine is taken up by any thyroid tissue not removed by surgery, including cancerous cells spreading to other body parts, such as lymph nodes. In addition to emitting electrons that destroy the tissue harboring the radionuclide, radioactive iodine emits photons suitable for imaging.
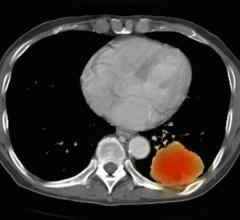
“Normal thyroid tissue as well as residual cancer cells concentrate radioiodine. Performed after ingestion of radioiodine, SPECT-CT provides three-dimensional images of the distribution of the radionuclide in the human body and is therefore used for staging this type of cancer,” said Torsten Kuwert, M.D., co-author of the article. “Incorporated at first treatment, SPECT-CT allows us to better stratify patients into treatment groups.”
In the study, 57 patients received radioiodine therapy. Afterwards, a SPECT-CT camera was rotated around the patients at a variety of angles to capture where the radioactivity was occurring. SPECT imaging can locate cells in the body that are not behaving normally, but does not provide the detailed, X-ray-like images that CT imaging can. The hybrid camera, however, is able to reveal both the malignant cell activity and the exact anatomical location.
“With SPECT-CT imaging, we were able to determine tumor spread much earlier than before,” said Daniela Schmidt, M.D., another co-author of the article. “Earlier detection will lead to earlier individualized treatment of this potentially deadly cancer.”
The researchers also reported that this information led to a revision of the original diagnosis in 35 percent of the study participants. The images reclassified as benign six of 11 lesions that had been considered lymph node metastases and 11 of 15 lesions considered to be indeterminate.
“Our data suggest that SPECT-CT should be used as a routine procedure in DTC patients at the first radioiodine treatment,” said Dr. Kuwert. “By upstaging or downstaging disease, this hybrid imaging tool may alter the management of more than one-third of patients with the disease.”
According to the American Cancer Society, DTC is the most common form of thyroid cancer and one of the success stories in the war on cancer. Since the advent of radioiodine therapy, it has been considered one of the more curable cancers. In 2009, about 37,340 new cases of thyroid cancer will be diagnosed in the United States. Of the new cases, about 28,410 will occur in women, and 8,930 in men.
Co-authors of “Impact of I-131-SPECT/Spiral-CT on Nodal Staging of Differentiated Thyroid Carcinoma at First Radioablation” include Daniela Schmidt, Attila Szikszai, Rainer Linke, Torsten Kuwert, Clinic of Nuclear Medicine; and Werner Bautz, Institute of Radiology, all from the University of Erlangen-Nürnberg in Erlangen, Germany.
For more information: www.snm.org

 February 15, 2024
February 15, 2024