Findings released on the final day of the Radiological Society of North America Scientific Sessions and Annual Meeting, RSNA 2023, showed that early detection of breast cancer, before symptoms are present, is key to survivability. After adjustment, there was a 66% reduction in the risk of breast cancer death among women who attended their five most recent screening mammograms, compared to those who attended none.
November 30, 2023 — Breast cancer mortality is significantly reduced when women regularly attend screening mammograms, according to research being presented on the final day of the Scientific Assembly and Annual Meeting of the Radiological Society of North America, RSNA 2023.
Robert A. Smith, Ph.D.
Early detection of breast cancer, before symptoms are present, is key to survivability. According to the American Cancer Society, women between the ages of 45 and 54 should get mammograms every year. Women who are 55 years and older can switch to every other year or continue with annual mammograms. Skipping just one scheduled mammogram could result in a more advanced breast cancer diagnosis, significantly impacting a patient’s chance of survival.
“The purpose of mammography is to detect breast cancer during the few years it can be seen on a mammogram, but before symptoms are apparent,” said study author Robert A. Smith, Ph.D., senior vice president and director of the American Cancer Society Center for Cancer Screening in Atlanta, Georgia. He added, “If a woman unknowingly has breast cancer and misses or postpones her mammogram during this time when she has no symptoms, but her breast cancer is growing and perhaps spreading, then the window for early detection will be lost.”
Even though regular mammograms are an important factor in early breast cancer detection, there are still many barriers that restrict women from receiving this preventative care, including access and work or family obligations.
“It is challenging to keep track of your schedule, and in the U.S., many women do not receive reminders. Further, for all of us, the obligations of work and family compete with our scheduled health care,” Dr. Smith said.
Dr. Smith and colleagues sought to identify the exact impact of missing even one mammogram.
The researchers obtained women’s screening history from oncology centers throughout Sweden for a period from 1992 to 2016. A total of 36,079 breast cancer patients were included in the study.
Using data from the Swedish Cause of Death Register, the researchers identified 4,564 breast cancer deaths among the patients included in the study.
The researchers then tracked all of the women’s participation in five or fewer most recent invitations for breast cancer screening prior to cancer diagnosis.
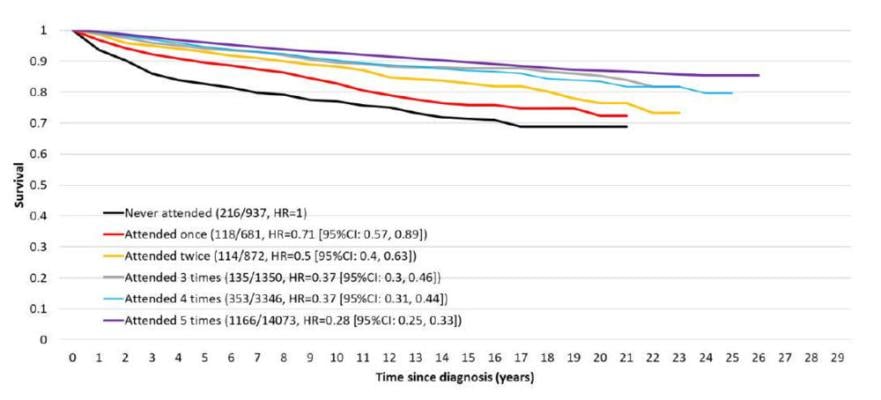
Women who attended all their invited screening mammograms had a survivability rate of over 80%. Women who didn’t participate in any screenings had a survival rate that ranged from 59.1% to 77.6%.
Women who attended all five screening mammograms saw a 72% reduction in the risk of dying from breast cancer compared to women who didn’t participate in any screening mammograms. Even after conservative adjustment for potential self-selection factors, there was a highly significant 66% reduction in the risk of breast cancer death.
“Women who attended all five previous mammography examinations prior to a diagnosis of breast cancer were nearly three times less likely to die from breast cancer compared with women who had not attended any examinations, and each additional examination attended among the five previous examinations conferred an additive protective effect against dying from breast cancer,” Dr. Smith said.
The researchers stressed that imaging facilities should prioritize getting patients in for screening at the earliest opportunity. This is especially important when women have to cancel their appointments. Facilities should reschedule these screening mammograms for the next earliest available appointment.
“These findings show that as much as possible, adherence to regular mammography screening is the very best insurance a woman has against being diagnosed with an advanced breast cancer that could be life-threatening,” Dr. Smith said.
Co-authors are Stephen W. Duffy, M.Sc., Amy Ming-Fang Yen, Ph.D., László Tabár, M.D., Abbie Ting-Yu, Ph.D., Sam Li-Sheng Chen, Ph.D., Chen-Yant Hsu, M.D., Peter B. Dean, M.D., and Tony Hsiu-His Chen, Ph.D.
For more information: www.rsna.org
Find more RSNA23 conference coverage here
Related Breast Density Content:
VIDEO: FDA Update on the US National Density Reporting Standard - A Discussion on the Final Rule
One on One … with Wendie Berg, MD, PhD, FACR, FSBI
Task Force Issues New Draft Recommendation Statement on Screening for Breast Cancer
Creating Patient Equity: A Breast Density Legislative Update
AI Provides Accurate Breast Density Classification
VIDEO: The Impact of Breast Density Technology and Legislation
VIDEO: Personalized Breast Screening and Breast Density
VIDEO: Breast Cancer Awareness - Highlights of the NCoBC 2016 Conference
Fake News: Having Dense Breast Tissue is No Big Deal
The Manic World of Social Media and Breast Cancer: Gratitude and Grief
Additional Breast Imaging and Related Content:
Single vs. Multiple Architectural Distortion on Digital Breast Tomosynthesis
Today's Mammography Advancements
Digital Breast Tomosynthesis Spot Compression Clarifies Ambiguous Findings
AI DBT Impact on Mammography Post-breast Therapy
ImageCare Centers Unveils PINK Better Mammo Service Featuring Profound AI
Radiologist Fatigue, Experience Affect Breast Imaging Call Backs
Fewer Breast Cancer Cases Between Screening Rounds with 3-D Mammography
Study Finds Racial Disparities in Access to New Mammography Technology



 December 08, 2025
December 08, 2025 









