Image courtesy of Volpara Solutions
December 11, 2015 — Researchers from Elizabeth Wende Breast Care (EWBC) demonstrated the importance of automated volumetric breast density to improving the performance of mammographic screening programs in two studies presented at the 101st annual Radiological Society of North America (RSNA) meeting. According to the researchers, the technology provides better understanding of which women have reduced sensitivity and are more likely to be diagnosed with an interval cancer.
Conducted by Stamatia Destounis, M.D., Andrea L. Arieno, BS, and Renee Morgan, RT, of EWBC, the studies were presented by Destounis as part of the Breast Imaging (Density and Risk Assessment) Session, moderated by Jennifer Harvey, M.D., of University of Virginia Health System.
“Breast density has been shown to be a significant factor in masking risk, and is a major factor in the reduced sensitivity of mammography. The visual assessment of density is subjective and may not provide reproducible results. This becomes more important as we design screening protocols and make decisions about adjunctive imaging for women with dense breasts,” said Destounis, attending radiologist at Elizabeth Wende Breast Care. “The results of these two studies demonstrate that automated volumetric data is very consistent and showed a strong linear correlation to mammographic sensitivity as well as predicting the risk of interval cancers. This needs to be confirmed by studies at additional centers, but these are very encouraging results.”
The study, “Quantifying the Potential Masking Risk of Breast Density in Mammographic Screening,” was designed to compare the current method of reporting on reduced mammographic sensitivity, using the visual American College of Radiology (ACR) BI-RADS density assessment categories, with quantitatively assessed volumetric breast density. The study included 774 screen-detected or interval cancers diagnosed at EWBC between 2009 and 2012.
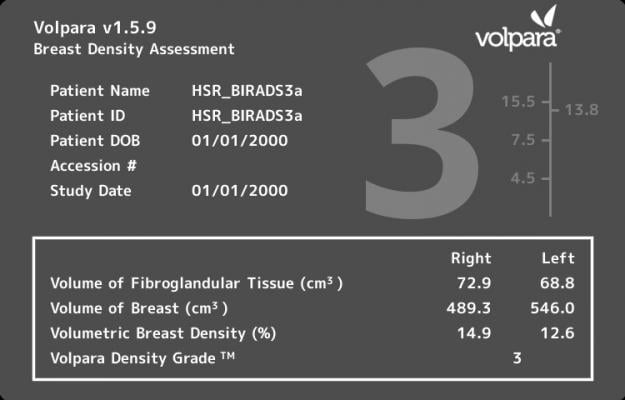
Breast density was assessed using both the visual BI-RADS 4th Edition and VolparaDensity, a commercially available software tool that automatically generates an objective measurement of volumetric breast density. The software categorizes density using the Volpara Density Grades (VDG), which are correlated to the BI-RADS density categories. Mammographic sensitivity was compared between the density assessment methods and within each VDG category, by dividing each category into high and low using the mid-point of each VDG threshold.
Results showed that volumetric breast density captures the potential masking risk of breast density more precisely compared to the widely used visual BI-RADS density assessment categories. The results also demonstrated that further sub-dividing each volumetric density category into “low” and “high” showed a strong linear relationship between volumetric breast density and sensitivity. While sensitivity was similar between low versus high in the low-density categories (VDG1 and VDG2), sensitivity decreased significantly between low versus high in the higher-density categories (VDG3 decreased from 87 percent to 75 percent and VDG4 decreased from 68 percent to 53 percent). With a linear relationship with mammographic sensitivity, the results suggest that volumetric breast density can be used to more accurately determine the effect of density on masking compared to the visual BI-RADS density assessment categories.
“The results indicate that within the BI-RADS 3 and 4 density categories there is a large range in sensitivity that is not being captured using the visual BI-RADS system which could impact the selection of women who would most likely benefit from supplemental imaging. The ability to use automated density measures to capture this masking risk may more accurately support screening protocols that are based on women’s personal breast density and other risk factors,” said Destounis.
The second study, “Volumetric Breast Density a Strong Predictor of Interval Cancer Risk” evaluated which patient factors — such as age, ethnicity, family history, previous hormone replacement therapy (HRT) use, menopause status and breast density — might best predict the risk of being diagnosed with an interval cancer. The study included 614 screen-detected or interval cancers diagnosed at EWBC between 2009 and 2012 and breast density was assessed using the visual BI-RADS 4th Edition and VolparaDensity Grades.
Results demonstrated that volumetric breast density is a strong independent predictor of interval cancer risk. Women with VDG4 were 3.9 times more likely to be diagnosed with an interval cancer than a screen-detected cancer compared to women with non-dense breasts (VDG1 and VDG2). Additionally, women in the highest density category (VDG4) compared to women in the lower density categories (VDG1 and VDG2) were 4.7 times more likely to be diagnosed with an invasive interval cancer than a screen-detected cancer. While visual assessments of BI-RADS density categories were also associated with interval cancer screening risk, volumetric methods were stronger predictors and due to its continuous nature, can be used to better identify women who might benefit from adjunctive screening.
For more information: www.ewbc.com


 July 30, 2024
July 30, 2024 








