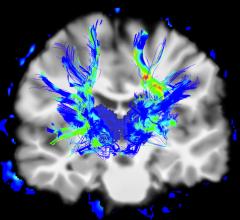
Research presented at RSNA 2022 by a team from The Martinos Center at Harvard University concluded that DCE-MRI reveals reduced pulmonary microvascular perfusion months after initial SARS-CoV-2 infection compared to age-similar healthy volunteers. Photo credit: Athinoula A. Martinos Center for Biomedical Imaging - Harvard University.
November 30, 2022 — Findings from four separate studies on long-term impacts of COVID-19 were presented during a “Cutting Edge: Long COVID” session in the Learning Center Theater on Nov. 30 during the 108th Scientific Assembly and Annual Meeting of the Radiological Society of North America (RSNA 2022) in Chicago, IL.
Solving the mysteries of Long COVID — with better diagnoses and treatment, and identifying radiological solutions to identifying lasting impacts — was a common theme among the researchers.
Peter Caravan, PhD, Professor of Radiology, Harvard Medical School, and Co-Director of the Massachusetts General Hospital (MGH) Institute for Innovation in Imaging (i3) in Boston, MA, detailed the way in which Dynamic Contrast-Enhanced CRI helped solve the challenge for patients whose standard tests appear normal, although their symptoms persist.
Noting that long COVID causes endothelial injury in the lung, and is an increasing health burden, Caravan said he and the research team, led by Iris Y. Zhu, PhD, were interested in looking at whether microvascular and endothelial dysfunction persist after resolution of acute COVID-19. In the study, “Dynamic Contrast-Enhanced MRI Detects Decreased Pulmonary Perfusion in COVID-19 Survivors,” researchers noted that dynamic contrast-enhanced (DCE) MRI has been used to explore pulmonary microvascular properties in patients with chronic obstructive pulmonary disease, lung cancer, and idiopathic pulmonary fibrosis. The team, part of the Athinoula A. Martinos Center for Biomedical Imaging - Harvard University, performed DCE MRI on participants with prior COVID-19 to assess for differences in pulmonary microvascular perfusion compared with healthy volunteers.
The team concluded that DCE-MRI reveals reduced pulmonary microvascular perfusion months after initial SARS-CoV-2 infection compared to age-similar healthy volunteers. Their results, Caravan noted, suggest that the DCE-MRI derived biomarkers are more sensitive to detect pulmonary microvascular abnormalities than pulmonary function tests. The results also provide insights into post COVID-19 microvascular pathobiology not otherwise available, and may have therapeutic implications in the treatment of SARS-CoV-2 infection.
“I think one of the most significant findings from our research was that using DCE MRI, we could robustly detect lung abnormalities that were not apparent on lung function tests,” said Caravan on the research he and his team conducted. He added, “These were subjects that self-reported with long COVID and had symptoms, yet their pulmonary function tests were appearing normal. So we found that we could detect this underlying pathology that was not seen using standard lung function tests.”
Sean Fain, PhD, Professor of Radiology-Division of Cardiovascular and Thoracic Imaging at the University of Iowa Health Care - Carver College of Medicine, presented findings from the “Assessment of Ventilation and Gas Exchange in Long COVID Using HP Xe MRI and Quantitative CT.” The team evaluated gas exchange and ventilation/perfusion ratio matching in survivors of acute COVID-19 infection with persistent fatigue and labored breathing. The interim analysis largely confirmed findings of persistent gas exchange abnormalities, as they found that significantly higher gas exchange heterogeneity was observed in Long COVID compared to healthy normal subjects.
Their conclusion: ventilation and gas exchange heterogeneity may be characteristic features of patients with Long COVID. Fain noted the clinical relevance, in that this longitudinal study of regional pulmonary function in long COVID using novel imaging will improve understanding of prolonged symptoms of fatigue and dyspnea. Elevated membrane gas ratio, a finding possibly suggestive of persistent lung inflammation or remodeling, early longitudinal data further supports this pattern.
From Pamukkale School of Medicine, Denizli, Turkey, Amet Yitik, MD, summarized the study he and others undertook, “Quantitative Chest CT Analysis (QCTA) of Patients with Post-COVID-19 Condition (PCC), in which 52 never-smoker patients with PCC, who underwent unenhanced chest exams and physical exams from June, 2020 to June, 2022. The purpose was to compare the QCTA results of patients with PCC and asymptomatic participants (AP) who had a history of hospitalization due to COVID-19. The researchers also aimed to compare CT analysis results with pulmonary function tests (PFTs).
The team’s conclusions were as follows, noted Yitik: 1) patients with PCC demonstrate a higher extent of post COVID-19 parenchymal changes and impairment of PFTs than asymptomatic participants (AP). 2) parenchymal abnormalities on CT were associated with the patient’s age, history of ICU admission, and length of hospital stay, 3) the PCC group had significantly lower trachea and main bronchial airway area than the AP group. According to the data, Yitik and his colleagues suggest that respiratory symptoms of PCC may be associated with post-infectious bronchiolitis obliterans.
Reporting on work done by the the Department of Radiology at Seoul St. Mary’s Hospital, College of Medicine, Catholic University of Korea, Kyongmin Sara Beck, MD, PhD, covered the findings from “Migratory COVID-19 Pneumonia in B-cell Lymphoma Patients Receiving B-cell Depletion Therapies.” The purpose, stated Beck, was to examine the clinical and radiological characteristics of COVID-19 patients with hematologic malignancy who show migratory airspace opacities on serial chest CTs with persistent COVID symptoms. The conclusion she shared was that COVID-19 patients with B-cell lymphoma who had recently received B-cell depleting agents may demonstrate migratory airspace opacities on serial CT with persistent symptoms, which could be interpreted as ongoing COVID-19 pneumonia related to prolonged viral shedding resulting from iatrogenic humoral immunodeficiency. Beck noted that being aware of this will help physicians make more accurate treatment-related decisions for patients.
For more information: https://www.rsna.org/annual-meeting


 July 30, 2024
July 30, 2024