May 21, 2008 - The Centers for Medicare and Medicaid Services (CMS) has initiated a national coverage analysis (NCA) for the use of screening CT Colonography for colorectal cancer, for which the public has 30 days to submit comments regarding the topic.
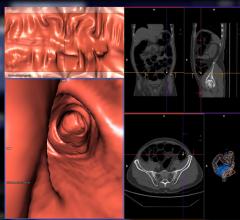
This NCA will evaluate the available evidence for screening CTC and determine if a national coverage determination is warranted. CMS currently covers colorectal cancer screening for average risk individuals age 50 and older using fecal occult blood testing, sigmoidoscopy, colonoscopy and barium enema. However, on March 5, 2008, the American Cancer Society, the U.S. Multi Society Task Force on Colorectal Cancer and the American College of Radiology issued new cancer screening guidelines, including a recommendation that computed tomography colonography (CTC) be considered an acceptable option for colorectal cancer screening for such individuals.
Neither the Medicare law nor the regulations identify the CTC test as a possible coverage option under the colorectal cancer screening benefit. However, CMS is allowed, under 42 CFR 410.37(a)(1), to use the national coverage determination (NCD) process to determine coverage of other types of colorectal cancer screening tests that are not specifically identified in the law or regulations as it determines to be appropriate in consultation with relevant organizations.
CMS considers all public comments, and is particularly interested in clinical studies and other scientific information related to the technology under review. CMS is also particularly interested as to the types of studies needed if the evidence is determined to be premature for coverage or if the appropriate frequency interval is uncertain.
CMS has urged that all public comments be submitted through the link below. Please do not submit personal health information in public comments. Comments with personal health information may not be posted to the Web site.
For more information: www.acr.org

 February 06, 2024
February 06, 2024 








