
August 26, 2019 — A team of Johns Hopkins data researchers is studying the economic and safety implications associated with the devices used to perform colonoscopies as a disposable version inches closer to widespread availability.
Gastroenterology researcher Susan Hutfless led a first-of-its-kind study published online in the BMJ journal Gut.1 The study reported that while disposable devices might lead to lower rates of post-colonoscopy infection, institutions that perform the procedure thousands of times per year might better benefit from improved disinfection methods of reusable scopes.
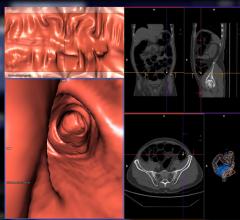
Today, colonoscopies are performed with reusable scopes, which are flexible, fiber-optic devices that are inserted into the anus and guided through the colon. The scopes allow endoscopists to examine patients for cancerous or precancerous conditions, as well as diagnose chronic disease. The nature of the devices and the microorganisms they encounter during use mandates rigorous cleaning.
In 2016, the U.S. Food and Drug Administration (FDA) approved a disposable colonoscope designed to be used only once. With the new devices on the horizon, Hutfless and her colleagues aimed to determine which centers, if any, might benefit from using them.
Only a small fraction of the more than 15 million Americans who had colonoscopies last year contracted infections from the procedure. But, as Hutfless noted in a 2018 publication, the rates of infection at facilities that perform a relatively small number of the procedures are far higher than previously believed. In that paper, Hutfless reported that rates of post-colonoscopy infection at facilities known as ambulatory surgery centers (ASCs) are more akin to 1 in 1,000, rather than the 1 in 1 million figure previously accepted in the field.
Given that the one-time-use scopes have yet to be introduced, Hutfless focused on the cleaning, capital and operating costs associated with the reusable versions currently available. Purchase, maintenance and cleaning costs per procedure range from $189 at centers that perform at least 3,000 colonoscopies per year, to $501 at centers performing 1,000 or fewer. When the cost of treating post-procedural infections is included, the numbers rise even higher, ranging from an additional $20 per procedure in high-volume, low-infection centers to almost $47 for centers with greater infection rates. The average cost of a hospitalization to treat a post-colonoscopy infection is more than $12,000.
Colonoscopies are recommended for people age 50 and above for routine cancer screenings. The procedures are performed under mild sedation in hospitals or ASCs. Hutfless’ research has shown direct correlations between the number of procedures performed at a particular center and the rates of infection.
“High-volume centers tend to have lower infection risks,” said Hutfless, adding that she and her colleagues attribute the lower risk to more experience and a faster turnover of colonoscopes. “It may not be cost-effective for high-volume centers to switch to disposable.”
The researcher said that certain low-volume centers could benefit from disposable scopes. “They may decrease device-related infection transmission and may prove cost-effective for some facilities, particularly those with low volume and patients with a high infection risk.”
She also pointed to the environmental impact that millions of throw-away plastic scopes would have. “That’s something that very much needs to be considered,” she said.
For more information: www.gut.bmj.com
References
1. Larsen S., Kalloo A., Hutfless S. The hidden cost of colonoscopy including cost of reprocessing and infection rate: the implications for disposable colonoscopes. Gut, August 2019. http://dx.doi.org/10.1136/gutjnl-2019-319108

 February 06, 2024
February 06, 2024 








