
February 16, 2009 - The Centers for Medicare and Medicaid Services is accepting comments until mid-March on its proposed decision to refuse coverage of computed tomography colonography (CTC) for colorectal cancer screening.
CMS said it is accepting comments on the cost effectiveness of screening CT colonography for the Medicare population if we were to alter our clinical decision.
“We are requesting public comments on this proposed determination…After considering the public comments, we will make a final determination and issue a final decision memorandum. As with all national coverage analyses, the public may submit comments or additional evidence that cause us to reassess our evidentiary review and arrive at different conclusions. If…we determine that CT colonography is clinically effective, then we would need to determine, using current or additional cost information, if CT colonography is cost effective. We are asking for public comment on the cost effectiveness of screening CT colonography for the Medicare population if we were to alter our clinical decision.”
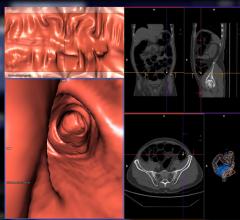
CMS announced its decision not to reimburse CT colonography on Feb. 11. 2009, stating, “The evidence is inadequate to conclude that CT colonography (CTC) is an appropriate colorectal cancer screening test.”
The proposal follows a November Medicare Evidence Development and Coverage Advisory Committee (MEDCAC) meeting, in which a majority of committee members expressed moderate confidence in the technology’s ability to determine with adequate specificity and sensitivity the presence of polyps greater than 10 mm, but less confidence in detecting smaller polyps. Committee members expressed even less confidence in the technology’s ability to increase overall cancer screening rates.
CMS determined that it did not appear that CTC had a similar ratio of cost per life-years saved, compared with optical colonoscopy. In the November meeting, representatives of the U.S. Preventive Services Task Force took the position that there is insufficient evidence to assess the benefits and harms of CTC.
When the Centers for Medicare and Medicaid Services (CMS) began its process of considering coverage of the technology in May 2008, it received 100 comments, 79 of which were in favor of adding CTC as a Medicare-covered benefit. The societies in support of coverage for asymptomatic, average-risk patients over age 50 years, which contributed their comments in the May 2008, included the American Cancer Society, American College of Radiology, American Gastroenterological Association, Medical Device Manufacturers Association and the Medical Imaging and Technology Alliance.
Because Medicare already covers screening tests known to lead to positive health outcomes, a new test should show evidence of increasing overall screening, according to the proposed decision. A new test should not lead to duplicative testing or switching from one test to another, and so far, there's nothing to say that CTC would lead to either of these scenarios, which would increase resource use, said CMS.
For more information: https://www.cms.hhs.gov/mcd/viewdraftdecisionmemo.asp?from2=viewdraftde…

 February 06, 2024
February 06, 2024 








