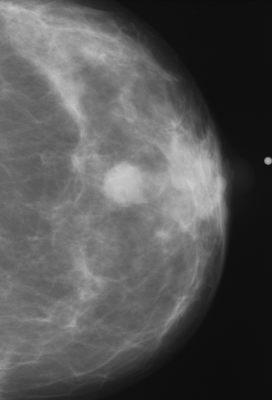
November 29, 2023 — A deep learning artificial intelligence (AI) model that was developed using only mammogram image biomarkers accurately predicted both ductal carcinoma in situ (DCIS) and invasive carcinoma, according to research being presented today at the annual meeting of the Radiological Society of North America (RSNA). Additionally, the model showed no bias across multiple races.
Constance D. Lehman, M.D., Ph.D.
Traditional breast cancer risk assessment models use information obtained from patient questionnaires, such as medical and reproductive history, to calculate a patient’s future risk of developing breast cancer.
“In the domain of precision medicine, risk-based screening has been elusive because we have not been able to accurately evaluate a woman’s risk of developing breast cancer,” said study lead author Leslie R. Lamb, M.D., M.Sc., a breast radiologist at Massachusetts General Hospital (MGH) in Boston. “Even the best existing traditional risk models do not perform well on the individual level.”
Traditional risk models have also demonstrated poor performance across different patient races, most likely due to the data used to develop the model.
“Traditional models likely have racial biases due to the populations on which they were developed,” Dr. Lamb said. “Several of the commonly used models were developed on predominantly European Caucasian populations.”
According to the American Cancer Society, Black women demonstrate the lowest 5-year relative survival rate for breast cancer among all racial and ethnic groups. This translates to a persistent 6% to 8% disparity in 5-year survival rates between Black and white women across all breast cancer types.
To accurately determine breast cancer risk, foster early detection and improve patient survival rates, it is important that risk models are developed that are applicable across different populations.
A deep learning AI risk assessment model developed using mammographic images alone can outperform traditional risk assessment models in future breast cancer development while also mitigating the racial biases seen in traditional models.
In the first study of its kind, Dr. Lamb and colleagues sought to assess the performance of an image-based deep learning risk assessment model in predicting both future invasive breast cancer and DCIS across multiple races.
The model’s performance was assessed by comparing areas under the receiver operating characteristic curve (AUC) with the DeLong test. The AUC score measures the predictive rate of the model on a scale of from 0 to 1. Multiple prior studies have estimated traditional risk model performance measured by AUC in the range of 0.59-0.62 for white women, with much lower performance in women of other races.
The multisite study included 129,340 routine bilateral screening mammograms performed in 71,479 women between 2009 to 2018 with five-year follow-up data. Patient demographics were obtained from electronic medical records, and instances of cancer were identified from the regional tumor registry.
The racial makeup of the study group included white (106,839 exams), Black (6,154 exams), Asian (6,435 exams), self-reported other races (6,257 exams) and unknown (3,655 exams). The mean age of the women was 59 years old.
The deep learning model consistently outperformed traditional risk models in predicting a woman’s risk of developing DCIS, which is early-stage breast cancer, and invasive breast cancer, which is cancer that has potential to spread.
“The model is able to translate the full diversity of subtle imaging biomarkers in the mammogram, beyond what the naked eye can see, that can predict a woman’s future risk of both DCIS and invasive breast cancer,” Dr. Lamb said. “The deep learning image-only risk model can provide increased access to more accurate, equitable and less costly risk assessment.”
The predictive rate of both DCIS and invasive cancer was 0.71 across all races. The AUC in predicting DCIS was 0.77 in non-white patients and 0.71 in white patients. The AUC in predicting invasive cancer was 0.72 in non-white patients and 0.71 in white patients.
“This is a particularly exciting domain for AI, as it demonstrates the opportunity to apply ‘AI for good’—to reduce well-known racial disparities in risk assessment,” said senior author Constance D. Lehman, M.D., Ph.D., a breast radiologist at MGH. “We are now poised to translate these findings into improved clinical care for our patients.”
Additional co-authors are Sarah F. Mercaldo, Ph.D., and Andrew R. Carney, M.S.
For more information: www.rsna.org
Find more RSNA23 conference coverage here
Related Breast Density Content:
VIDEO: FDA Update on the US National Density Reporting Standard - A Discussion on the Final Rule
Creating Patient Equity: A Breast Density Legislative Update
AI Provides Accurate Breast Density Classification
VIDEO: The Impact of Breast Density Technology and Legislation
VIDEO: Personalized Breast Screening and Breast Density
VIDEO: Breast Cancer Awareness - Highlights of the NCoBC 2016 Conference
Fake News: Having Dense Breast Tissue is No Big Deal
The Manic World of Social Media and Breast Cancer: Gratitude and Grief
Related Breast Imaging Content:
Single vs. Multiple Architectural Distortion on Digital Breast Tomosynthesis
Today's Mammography Advancements
Digital Breast Tomosynthesis Spot Compression Clarifies Ambiguous Findings
AI DBT Impact on Mammography Post-breast Therapy
ImageCare Centers Unveils PINK Better Mammo Service Featuring Profound AI
Radiologist Fatigue, Experience Affect Breast Imaging Call Backs
Fewer Breast Cancer Cases Between Screening Rounds with 3-D Mammography
Study Finds Racial Disparities in Access to New Mammography Technology



 April 17, 2025
April 17, 2025 







