Herman Oosterwijk, MS, MBA is president of Aubrey, TX-based OTech Inc., which specializes in healthcare training and consulting.
On a recent road trip to Arizona in my RV, I noticed that the dashboard indicator for the engine temperature did not function. My wife urged me to stop at a dealer to have it checked. After about a half-hour wait, the mechanic called me to look at what he found: A squirrel had apparently gotten into my engine compartment, made a nest and in the process chewed my indicator cable as well as one of the spark plug cables. He asked whether I had noticed the degradation in performance and poor fuel mileage running on five instead of six cylinders, but, as a matter of fact, I had not.
Why this story? Well, I have met with several PACS users who are unaware that their PACS is demonstrating poor fuel consumption — they have several people spending unnecessary time and effort, unaware that a tune-up could make a major difference. So, what are some of the areas that you might be looking for in a PACS tune-up?
Workflow Improvements
When is the last time you did a reassessment of your workflow? Are there unnecessary steps being performed? Could you replace some of these steps with an automated process and/or upgrade?
When I look at a system operation, I always take the Integrating the Healthcare Enterprise (IHE) profiles as a baseline or “gold standard.” At one institution, the PACS administrator used to spend about one or two hours every day manually comparing all the PACS studies with a RIS-generated list to ensure that none of the studies were lost for whatever reason. These reasons could be misidentification or improper selection from a work list by a technologist, forgetting to send the study from the modality, a modality occasionally dropping a connection and, therefore, sending incomplete studies, and so on. The administrator told me that he asked his IT colleagues to write a script to automate this comparison process and reduce the verification process to 15 minutes. However, he was unaware of the fact that there are transactions defined by IHE and implemented at most new modalities and PACS that exchange the status information between modalities and PACS, such as Modality Performed Procedure Step (MPPS) and Storage Commitment (STC), and would have eliminated the manual process completely.
Some of the institutions might actually have these features available, or even worse, have paid extra money for these features and are not even utilizing them. At one site, for example, I looked at the details on the purchase orders and discovered that the institution had spent a significant amount of money to have these options at their modalities, and that the service engineer had not bothered to switch them on. Remember, one needs these to be facilitated at the PACS and RIS as well as at the modality. At another institution, they had paid for this feature to be available at the PACS, and it was not configured properly, hence, it was not operating. Therefore, an assessment of your workflow against the IHE profiles definitely makes sense.
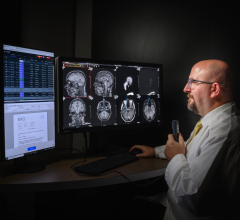
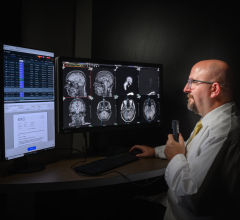
Image Display Integrity
When I give talks about image quality, I always ask the audience when they last calibrated their monitors. The answer ranges from one to six months. Fortunately, new diagnostic monitors have automatic calibration built in; however, older monitors and some of the lower cost models still require manual calibration. Because of the gradual nature of performance degradation, it is hard to notice the difference until the calibration is performed; it then becomes clear that there is more detail to be seen. Your calibration process and procedures might need to be revisited.
Image Quality Procedures
I talked with a radiologist at one site and asked his opinion of the recently installed PACS. He said that in 95 percent of the cases he thought that the image quality of his standard procedures was superior, however, in some cases there was a lack of detail in the black area. He did not realize that images are processed at the CR according to the “95 percent” rule, which is, in most cases, the image processing works fine, but in 5 percent of the cases there is a possibility for the data to be “clipped.”
One can compare this with making a print of a photo from your camera. The negative has more information in it, and the resulting look depends on the setting on the development machine where you get your prints done. The solution was simple — merely having a technologist perform a QA step to make sure the images showed all the information, and, if needed, reprocess an image at the CR/DR to optimize the image quality.
Dose Creep
Some of the PACS tune-up components do not affect the operation or efficiency, but impact patient care. Because of the CR/DR detector characteristics, which have a linear response with regard to the X-ray energy instead of the traditional “S-curve” for regular film, it is hard to detect whether an image was created by using too much X-ray energy. CR/DR is very forgiving, and especially when making portable X-rays, a technologist could easily overexpose the patient. Each CR image has a dose indicator that has a different name for different CR manufacturers. Whatever the name, the value should be within a certain range to make sure there was an optimal usage of the latitude of the CR detector/plate. There should be a QA process in place whereby images that were created with values outside this optimal dose range trigger an automatic retake by the technologist.
System Performance
System performance is relatively hard to quantify and measure. It usually starts with complaints from users that the “system is slow.” There could be several reasons for this. It could even be related to the weather conditions.
In one case, the radiologist was reading images from an adjacent facility that was connected with a high-speed microwave connection between campuses, which would slow down during heavy rain. I often hear of performance impact because the IT/networking department changes the configuration of their network, (e.g., changes router settings by which a certain link suddenly is downgraded, or maybe they install a firewall that is scanning all incoming images from outside a clinic). These are good reasons for you to make sure you closely collaborate with your IT colleagues and follow their changes and updates closely, while monitoring your system performance constantly.
Reject Analysis
Here is another potentially “hidden” issue. In the analog film world, one could just look at the waste bin to see how many films were rejected. In the digital world, one needs to make a concerted effort to identify those images that were rejected, identify the reason, perform an analysis and implement process improvements to minimize these rejects. Rejects because of patient movement are hard to eliminate, however, proper instruction of the patient through training (“Please hold your breath and don’t move”) might reduce these. This also helps identify technologists that create a high percentage of image rejects due to mispositioning and improper exposure, making them good candidates for re-training.
Misidentification
When looking at some of the images in the database of a PACS at one site, I noticed that the patient information was not correctly encoded in the image header. Further investigation showed that the data was entered manually by the technologist because the modality worklist was not yet installed.
In this case, I found that about 30 percent of the database records in the archive had some type of error, potentially impacting or even preventing retrieval of the images. This was the most extreme case I have ever seen, but in many sites, an error rate of three to five percent in the database is not uncommon. Unfortunately, because many of the patient records are never retrieved, these errors go often unnoticed, until one does a data migration of the archive. Suddenly, all of these images show up that were incorrectly or improperly identified. Therefore, the golden rule is to never let your archive integrity slip and keep a good eye on it. Fix errors immediately, and perform regular maintenance and checks to ensure that your data is in a good shape.
These are the most critical areas of a PACS where a tune-up could have a major impact. Unfortunately, most users do not realize that their system is not running at maximum capacity, and the only way to know that is to perform a regular “check-up.” In most cases, this can be done by internal staff, with the PACS administrator playing a pivotal role. If you don’t have the expertise in house, it might make sense to take your system to a shop that has experience with this type of tune-up, in other words, work with a PACS consultant. In either case, there is a potential big payback, resulting in higher efficiency and the potential for better mileage from your PACS, which could make a big difference to your bottom line.


 February 03, 2025
February 03, 2025