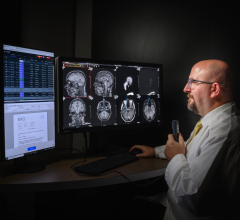
Eliot L. Siegel, M.D. is the professor of Diagnostic Radiology, director at Baltimore Veterans Affairs Medical Center Radiology and associate vice chairman for Informatics.
The “one-size-fits-all” approach to the radiology workstation no longer suits the radiologists’ needs. While vendors are racing to add more features and devices designed to raise the level of the radiologists’ performance, solutions lag behind in a field where technology is constantly evolving.
Larger volume datasets, fewer available radiologists and the need for remote and enterprise-wide access is changing the landscape of radiology reading. Many options for technological support exist, but the question is – what tools do radiologists want? The real challenge for the industry is to understand the radiologists’ mental workflow and simplify it through intuitive tools, so that the radiologists can focus on their principal task – analyzing images.
“The bottom line about workflow is making sure the radiologist spends as close to 100 percent of her or his time interpreting images as possible rather than doing the many other things that the current technology requires us to do in the process of image interpretation,” indicated Eliot L. Siegel, M.D., professor of Diagnostic Radiology, director, Baltimore Veterans Affairs Medical Center Radiology, associate vice chairman for Informatics.
Changes in Information Flow
The flow of data in and out of the radiologist workstation as well as changes in referral patterns have modified the tasks that radiologists perform, and in turn the way they think about their work.
If you consider clinical data, radiologists need to access more clinical information than what is available on the requisition. However, a by-product of PACS is that the ordering physicians are no longer going to the radiology department to retrieve images and, at the same time, are not providing the radiologist with additional information on the patient. Subsequently, many radiologists access the main hospital system to infer more clinical data on the patient to support in interpreting the exam. In this case, the stream of information to radiologists has been shut off, and they must seek out a new source.
The role of the radiologist with the referring physician – the radiologist’s true client – is also evolving due to advancements in technology. As referral patterns become more complicated, the radiologists’ challenge is to provide image data to the referring doctors in the most efficient manner.
“Implicit in the concept of the radiology workstation is the radiologist is going to read an image and do a narrative report. Increasingly, as these images become richer and the questions become more complicated, part of the radiologists’ job is to provide an image downstream as opposed to just a report. So what are the tools to allow annotation of an image for downstream delivery?” asked Donald W. Rucker, M.D., vice president and chief medical officer, Siemens Medical Solutions USA. “These workstations are becoming the workstation light for the ordering doctor. So a neurosurgeon or orthopedist or an ER doctor may also need a radiology workstation, but without all of the features, the buttons and the hanging protocol. The radiologist will want to control that since its part of their service to their customer base.”
Clearer Communication
Communication is also critical to servicing the referring physicians and for ensuring quality patient care. Many radiologists would like to add to their wish list a mechanism that confirms the receipt of a report. “The primary tool that we lack is a method to communicate radiology results and receive an acknowledgement of receipt of those results and a follow-up about any actions that were taken as a result of the report,” noted Dr. Siegel. “Our clinicians use a variety of different communication devices including fax machines, e-mail, voice mail, cell phones and pagers. In the absence of a unified communication strategy by our enterprise, a system that could keep track of the way each clinician wants to be contacted and how they can acknowledge that communication would be very important for us to close the communication loop with our clinical colleagues.”
Even mundane issues such as who the cross-coverage is for the doctor who ordered the film could be simplified with an integrated tool to contact referring doctors. David L. Weiss, M.D., clinical head of Imaging Informatics, Geisinger Medical Center suggests that, “[a] better system would be one that is built into the reporting process of communication software where I can assign a level of severity to each report and have the software contact the referring physician using his or her preferred mode of communication.” Ideally, user preference will dictate every aspect of the workstation, including hanging protocols, worklists, user interfaces and data filtering. But before designing and building a new model, vendors need to look closely at the radiologists’ mental model.
The Intuitive Model
It is one thing to ask the radiologist – what are you doing? But it is another to ask – what are you thinking? “This is the difference between good to great user interfaces,” according to Dr. Rucker, who emphasizes the importance of making radiologist workstations as intuitive as possible.
“As a general metric on intuition when you design these computer screens, you try to get into the head of the user and truly understand what is their thought process. What is the user’s mental model of the task?” said Dr. Rucker. “When considering easy-to-use navigation, you need a synergy between screen flow and the user’s mental model. It takes a lot of interviewing to understand what the decisions are that they are making when they look at the screen. What are the analyses that are going on in their head? It’s what am I thinking, not what am I doing.”
A daunting task, yet critical to developing a system is the interviewing process. The vendor must conduct a series of nterviews in an attempt to capture an understanding of the radiologists’ stream of consciousness while reading. The next step for engineers is to keep up with the mental synapses through shortcuts.
Key Short Cuts
The more intuitive the software, the less dependence there is on mechanical devices such as the mouse, keyboard or microphone. “As with any machine interface, it is the user preference that dictates the usefulness of the software,” pointed out Reuven Shreiber, M.D., vice president of Clinical Applications, Algotec, a Kodak Company. “Thus there are the ‘mouse’ users that want everything to be operated by the mouse, and there are some users who prefer shortcuts.” Shortcuts are key to simplifying the workflow, and the keyboard may be the first apparatus to be cut from the radiologist workstation.
“In general, any icon click, keyboard stroke or pulldown menu should be avoided,” said Dr. Weiss. “The reason for this is that these remove my eyes from the images and break my concentration. All PACS and dictation control must be performed without the need for visual input. The problem with the keyboard is that to be used properly it requires two hands. This leaves no hands for mouse or dictation control or else requires me to look away from the images to find a particular key.”
As an alternative to the keyboard, Dr. Weiss says that for CT and MR readings he uses the shuttle Pro control device in his left hand and a five-button mouse in his right hand. “I can program 15 buttons on the shuttle Pro in addition to the mouse buttons for PACS and dictation control. I also use voice commands for the speech recognition dictation system. I use a headset microphone exclusively keeping both hands free for the mouse and shuttle Pro.” Dr. Weiss added, “Ideally we should be designing the hardware and software controls together. This is what Apple did with the iPod – what I consider the apotheosis of an ideal user interface.”
Scheduled for release this September is a study conducted by GE Healthcare and the aforementioned Dr. Siegel in which they use a tracking system to monitor the usage of a PACS workstation to see what buttons people are using, what areas of the image the mouse most often hovers over and what functions are used repeatedly. “Hopefully, what we will learn from the study is if there are 15 different buttons up on the screen, and they are only using four of those buttons for a majority of their procedures, then why not just show the four buttons that are being used repetitively,” explained Mark Morita, Next Gen Workstation Lead, Imaging and Information Systems, GE Healthcare.
Filtering Data
While tracking promises to reduce the number of steps to perform a task, intuitive programming will diminish the number of devices the radiologist is required to handle, as well as the number of decisions needed to be made. Predefined filters can automatically sort a worklist according to user preference, so that, for example, STAT studies appear at the top of the list, and hanging protocols can select, for example, relevant priors.
“The ultimate PACS workstation software should learn and anticipate a user’s next command,” indicated Dr. Weiss. “This is starting to be done to some extent with reading protocols. For example, if I always move from viewing a body CT scan first in the soft tissue window and then in the bone window, this should be seamlessly included in my protocols. If there are other sequences that I am performing, the software could ultimately learn and incorporate these for me as well.”
One area where radiologists frequently set protocols is to display large-volume CT slices in stack mode. “I prefer to view on one screen a reformatted presentation of the 3-D dataset – MPR viewer, so I can dynamically scroll through the study, while on a second monitor receive the original images in a stacked mode in order to verify that I review all of the available information. This is performed automatically on some PACS while other systems require additional work on the modality,” said Dr. Shreiber.
As intelligent software evolves, the graphical user interface will develop a personality based on the individual user and display tools specific to exam type and physician specialty. “There is too much clutter on the screen and the tools that are unrelated to the mission should be off the screen,” said Edward M. Smith, ScD, FACNP, professor of Radiology, Department of Imaging Sciences, University of Rochester. “When a person logs in and selects a study type, like CT, the tools that are most relevant to working with the CT should only be up there.”
Sifting Through the EMR
Filtering data will become increasingly important to productivity as image datasets become even larger and as PACS becomes integrated with the EMR.
“Advanced visualization software, including 3-D and 4-D capabilities are, in my opinion, essential for routine interpretation of all imaging studies and should be part of the image interpretation process” and “integrated with the PACS,” noted Dr. Siegel. As 3-D and 4-D rendering becomes standard in workstations, these highly dynamic images pose a whole new set of questions. “The physician may ask what organs do I show; how do I colorize these vessels; what do I keep or cut out of the picture?” indicated Dr. Rucker. “It is an example of when you have so much data no one person can process all of that. When you look at future workstations with increasing volumes of data, the one role of the workstation is to filter data and look at the data that is most important. It may be implicit or explicit; filtering it by displaying it in ways that allow you to answer the clinical question that is being asked.”
As hospitals and clinics implement enterprise-wide software solutions, such as PACS, and digitize medical records, radiologist and other physicians will access these systems to gather clinical data on the patients. Once again, the high volumes of information require a filter.
“I need access to highly filtered clinical content at the workstation. This can be either within my PACS or my communication software. By ‘highly filtered’ I mean that I cannot be constantly searching through the EMR to find a particular lab value. I need software that will anticipate that when I am deciding on a particular CT protocol, the most recent BUN and creatinine are the lab values that are most pertinent,” said Dr. Weiss.
“Likewise, my clinical colleagues should not have to download and search through a 1000 slice CT dataset. Their queries in the EMR should allow hem to immediately access my report with hyperlinks between keywords and thumbnail images. A double click on either the thumbnail or linked word would display only the pertinent, annotated images from the CT scan.”
Browser-Based Workstations
Another impact from both the exchange of image data and 3-D and 4-D rendering is a move to a browser-based workstation. Internet-based software is faster and ultimately less expensive. “Large volume datasets required for 3-D and 4-D image review will force a change from client-based to server-based image rendering in order to minimize the time required for image review, to maximize the power available at the client workstation, to keep costs reasonable and to eliminate the need to upgrade both hardware and software on PC’s throughout the imaging department and the enterprise,” said Dr. Siegel.
Dr. Rucker concurred, pointing out that “in an internet era where these images are shipped all over the world to referring docs for telemedicine, most imaging workstations are in fact going to be virtual. They are going to be a browser.” He added, “The docs who are referring business to the radiologists will be working on a browser instead of a 2 mega-pixel screen. The radiology departments are increasingly distributing images into heterogeneous environments, some of which are dedicated workstations and others of which are browsers.”
A New Vision
Many new technologies introduced to the radiologist workstation have created a new vision of how the reading room will look. To illustrate this image, GE Healthcare has designed a model NextGen workstation in which new devices, many adopted from other industries, are embedded into a new vision of the radiology workstation. Some of the tools include:
Graffiti PACS - leveraging the Graffiti used for the palm applications, this tool allows simple, handwritten gestures on the Wacom tablet to interact with the application. Rather than having to point and click on a tool and then affect a certain area on the screen of the Wacom tablet.
“So rather than having to use your eyes to find an icon and then bring a magnifying glass to the area, you can actually look away and focus in on the diagnostic interpretation. Your eyes are being used for scanning the image for pathology or anomalies and your hands are more interacting with the application itself,” said Morita.
Voice Command - voice commands embedded in 3.0 Centricity allow the user to zoom in, zoom out and move to the left and right of the next image. “What we have done,” said Morita, “is we have assigned different keyboard shortcuts to a variety of different functions and tools.”
Jog & Shuttle - created by Contour Design, the system was designed for video editors to sequence very quickly through an image or a video sequence to edit and cut, copy and paste, fast forward, rewind and more.
Space Ball - a tool that enables CAD users to easily navigate 3-D objects, rotate and zoom in on images with a rubber ball placed on top of a flat mouse device. “You can rotate around the x-axis, the y-axis,” said Morita. “It would essentially feel like holding the actual object in your hand and then affecting it.”
Gesture Control - gesture control, created by Microsoft research, uses Firewire Web Cameras to capture hand motions from five to 15 feet in front of the display. Users can motion on the screen to point the cursor, and then use voice command to affect the screen itself by saying zoom in, zoom out, etc.
Instant Messenger – allows users to send text messages to the referring physician immediately online or to a cell phone.
Desktop Sharing – enables physicians at different PACS stations to share an anomaly or pathology on an exam. Users can view from a hand-held smart phone or ultramobile PC in real time, similar to WebEX or same time desktop sharing applications.
Eye Tracker – created by Philips FIMI, infrared lights are illuminating and a camera tracks the direction of the user’s gaze from those illuminations, then guides the cursor’s motion on the screen.
The vision of the ideal workstation may be crystal clear to many radiologists, while the real challenge is for the industry to simplify the radiologists’ mental process “through ergonomics, input devices, simpler means of user interaction and embedding application-training,” said Morita. Could it be that the vendors are finally seeing the light at the end of the workstation?



 November 29, 2025
November 29, 2025