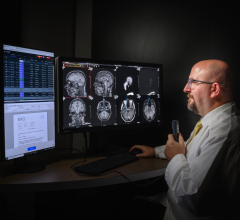
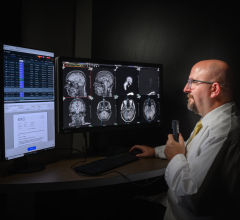
Dr. Steven Matchett at Lehigh Valley Hospital and Healthcare Network says telemedicine allows nurses to act on their concerns immediately.
It's 2 a.m. in a Fort Wayne, IN, hospital and a critical care nurse is concerned about one of her patients. He just doesn't look right, but she can't see anything that is completely out of range on his various monitors.
In most ICUs, the nurse would have to wonder whether to awaken the doctor on call or wait until the doctor makes his rounds at about 7 a.m. Fortunately, this hospital has an intensivist on duty, and she asks him to take a look at her patient.
About an hour later, in Jefferson City, MO, a nurse is worried about a falling respiratory rate of a patient and also needs the services of an intensivist.
In both cases, the intensivist who was called was the same person — and he was in St. Louis.
Welcome to the world of ICU telemedicine — a revolutionary change in how patients in ICUs are being monitored 24/7 in hospitals across the country.
“In most hospitals in the U.S. today, at 2 a.m. the goal of the ICU is simply focused on keeping the patient alive until the sun comes up and staff doctors are in the hospital,” said Stephen Matchett, M.D., chief of Clinical Care Medicine at Lehigh Valley Hospital and Healthcare Network, Allentown, PA.
With the use of ICU telemedicine, intensivists — in short supply nationally — can be on the scene, even though they may be hundreds of miles away, thanks to developments in electronic medical record keeping and telemedicine gadgetry such as high resolution, remote-controlled cameras and alarms.
“The nursing staff was skeptical about the system when we first set it up in 2004,” said Dr. Matchett. “But within two months, every nurse on duty had her own story of how having the 'second set of eyes' available helped solve a problem with a patient.”
The problem for nurses in the ICU is that if they wake someone up at 2 a.m., there had better be a good reason, he said. In the case of a “funny feeling”, the nurse may wait until she checks on the patient again. In that scenario, Dr. Matchett said, important, critical time could be lost.
“The nurses are now the strongest advocates of the system,” Dr. Matchett said, who oversees the telemedicine program responsible for 104 ICU beds in nine different hospitals in the Lehigh Valley system. Intensivists are at the patient bedside for 10 to 12 hours a day, but from 7 p.m. to 7 a.m. the system is turned over to intensivists in the ICU telemedicine group.
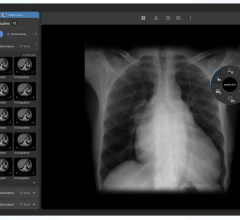
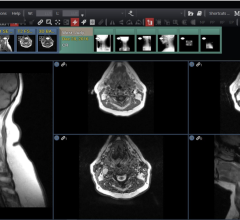
The system uses a platform based on the iMDsoft (Needham, MA) electronic medical record that gives the intensivist access to all the patient's records at the click of a mouse. The information can be displayed on a bank of eight monitors that also show the patient's current vital signs, X-ray or other digital scans and a live view of the patient on a camera in the ICU. The system also includes automated alarms that sound at both the hospital and in the dedicated ICU monitoring complex.
Dr. Matchett said the system at Lehigh Valley has interfaces that connect the electronic medical record with the patients' ventilator use, dialysis use and medication prescriptions to give doctors that information at bedside and at the ICU telemedicine suite. Computerized physician order entry systems eliminate most use of paper orders, which also tends to eliminate errors in reading physician scrawls.
“Since we began ICU telemedicine we have been able to see major benefits that are cost saving and life saving,” Dr. Matchett said. The length of stay in the ICU for low severity patients has been reduced from 1.8 days to 1.3 days, he said. Among ICU patients with moderate severity of illness, the hospital mortality has decreased from 15 to five percent of patients.
“Another way of expressing that is that it now requires us to treat just 10 patients in order to save one life,” Dr. Matchett said.
Lives saved
In Atlanta, Lynn Peterson, manager of media relations at St. Joseph's Hospital, said, ”We have just been operating ICU telemedicine for two months and we already have documented at least three lives that were saved because of the system.”
In one case a patient had somehow managed to dislodge ventilation machinery.
“The VISICU (Baltimore) system noted that the patient's heartbeat had increased but respiration had decreased and sounded an alert. That is something that can be overlooked in a busy critical care facility like ours at St. Joseph's Hospital. The critical care nurses can't be at a patient's bedside 24/7, but the monitors can be.”
At St. Joseph's, 48 patients are being monitored with the VISICU system. During the day, the hospital's 12 intensivists are on rounds with the patients, but after 5 p.m., the patients are monitored in a dedicated suite on the hospital campus about a half block from the patients.
Two critical care nurses are in the hospital with the patients, while the intensivists constantly monitor data screens and can use a high-resolution camera to take a closer look at specific patients who maybe in trouble.
“The doctors who work in the ICU telemedicine suite liken it to working in an airport control tower,” Peterson said. “There has been a real comfort level with the system. The physicians are confident that their patients are being monitored. There is a lot of feedback and interplay between the intensivists and the admitting doctors.
“This is a new model of care. The nurses have a second pair of eyes that can give them a second opinion,” Peterson said. “We are seeing that our patients are in and out of the ICU faster. It does have an effect on costs as well.”
“We have mainly cardiac patients, gastrointestinal patients, cancer patients — people who are very sick, so a large proportion of our beds are dedicated to the ICU,” Peterson said. The hospital is planning on adding six more beds to the eICU system this summer. “We have nine affiliated hospitals that we are planning to roll into the system as well.”
In St. Louis, Mary Jo Gorman, M.D., MBA, chief executive officer for Advanced ICU Care, St. Louis, MO, said her systems have been caring for patients in 72 ICU beds in seven facilities in hospitals and clinics in Jefferson City, MO; Wausau, WI; and Fort Wayne, IN, since January 2006.
“We need to have a clinician at each of those facilities with the expertise to put in a central venous access line and to intubate a patient,” said Dr. Gorman. “After that, just about everything else can be accomplished between the intensivist and the critical care nurse. By using telemedicine, we are able to bring the expertise of the intensivist to the local community 24/7.”
Compelling results
Convincing doctors to turn their patients over to other doctors who are a long jet flight from bedside wasn't immediately accepted.
“Physicians are not early adopters. None of us like change,” said Dr. Gorman, but the results have been convincing.
In the VISICU system used in her hospitals, the intensivist sits in front of six monitors that detail patient history and his or her current condition. An InTouch robot (InTouch Health, Santa Barbara, CA) can go to the bedside and get close enough to the patient and send back pictures sharp enough for doctors to monitor a patient's pupils reaction to light.
“The resolution is amazing,” Dr. Gorman said.
The intensivist eICU also helps nursing performance.
“In an ICU it is possible to forget to do routine procedures,” Dr. Gorman said. “For example, there are several steps that need to be accomplished to help prevent pneumonia when a patient is on a ventilator. We found that our rate of deep vein prophylaxis of patients on ventilators was at 70 percent and we were at 75 percent accordance with standards in elevating the head of the bed of the patients before we went to ICU telemedicine. In the third quarter of 2006, we achieved 100 percent compliance because the system records everything going on in the ICU, and nurses and doctors can be reminded to perform procedures that may be forgotten in an emergency or during consultations with patient families.”
More important, Dr. Gorman said, “since we instituted ICU telemedicine, our nursing turnover has decreased 67 percent. Nurses no longer have to worry about whether they should call a doctor. They know the doctor is just a push of a hot button away and someone can take care of a patient. A lot of the stress of working in the ICU environment is relieved by ICU telemedicine.”
In one case, she said, a nurse noticed a bit of swelling at the groin incision site of a patient who had undergone a percutaneous coronary intervention. Without an eICU, she might have not done anything until the next time she checked on the patient. In this case, she asked the intensivist on duty to electronically look at the patient's leg. The intensivist immediately recognized that the patient was bleeding under the skin, reduced blood thinners and contacted the surgeon and cardiologist to check on the patient, whose condition was quickly stabilized.
“In the routine ICU, that nurse might have waited another 30 minutes or an hour to have seen the patient again and then would have had to call in a doctor, who would have then called the surgeon. A couple of critical hours could have passed, and the outcome might have been tragically different,” she said.
The ICU telemedicine wave is moving worldwide. “The telemedicine ICU is the future of critical care medicine,” said Antonio Mas-Ordeig, M.D., head of the ICU at University Hospital Clinic, Barcelona, Spain.
“We don't have these systems in place yet at our hospital, but we know they are coming and we are excited about them,” Dr. Mas-Ordeig said.
“These systems have the promise of being able to monitor our patients 24 hours a day with a specialist in intensive care. I think they are going to be life saving.



 July 25, 2024
July 25, 2024