Allen Scales, vice president, Corporate Strategy, Emageon, Birmingham, AL
Choosing the ideal picture archiving and communications system may seem like a pipe dream to a clinician or administrator at an outpatient care facility. Sometimes those ideal desires may be unrealistic for a variety of reasons so “optimal” becomes the next standard of comparison.
Or does it?
Doctors want to focus their attention and time on serving patients at the expense of business decisions, which in today’s healthcare environment is more of a luxury than standard operating procedure. Administrators simply want tools to move images and data from point to point to operate their outpatient care facilities more efficiently without having to invest too much effort and time in disruptive technology.
Outpatient Care Technology magazine wanted to help its readers make some sense out of the process with can’t-miss PACS purchasing strategies. So we asked key executives at some of the leading PACS companies one simple question about evaluating and acquiring the optimal, if not ideal, PACS.
If an outpatient care facility clinician or administrator came to you for advice on how to evaluate and select the right PACS (e.g., business or clinical) what five actionable tips would you give them (in addition to promoting your products) to help them choose the optimal, if not ideal, system for them? How can “ideal” be realistic?
Anthony C Toppins M.D., radiologist, CIO, American Radiology Associates, Dallas
1. Strongly consider a true Web-based product that has the fewest ‘moving parts’ possible for ease of administration. This is critical for imaging centers and small hospitals without a large IT infrastructure and support staff. Ideally this may be as streamlined as a single production server and backup server. The Web-based products are often ideally suited and tailored to imaging centers and smaller community hospitals and can be deployed easily to multiple locations.
2. Do not forget the dictation piece! Too many evaluations focus on the PACS but select a dictation product as an afterthought. In many ways the dictation system is as important as the PACS.
3. As with any product purchase, select a system with the users in mind. If you pick an easy-to-use intuitive interface that utilizes drag-and-drop thumbnails and familiar Windows functions your radiologists, referring physicians and ancillary staff will be more enthusiastic about the new system. That ultimately improves productivity and morale. Ideally consider a system that has the same user interface no matter how a user is accessing it whether from a CD viewer, over the Web or on the LAN. This is the case with Web-based products such as Amicas.
4. Talk to other customers and your peers before making a purchase. I discuss PACS with other radiologists every week and learn something every time. The two best ways to evaluate products are to use them yourself and to talk to other users who have more experience with them. Demos are just that –demonstrations. Other users will give you real-world experience that isn’t ‘canned’ or ‘controlled.’ A demo simply doesn’t reproduce the real conditions of any radiology practice or department.
5. Put as much emphasis on workflow evaluation as you do on the viewer functionality. Most PACS demos are focused on the workstation viewers. While this is an important part of a PACS, I would argue that some degree of parity is being achieved with respect to the viewing software. However, there is a dramatic disparity in the workflow as it relates to the worklist functionality and the way the system performs under various conditions such as gigabit LAN versus a slower DSL connection. Worklists like the Amicas real-time worklist allow numerous radiologists to work together on the same list without duplicate dictations and wasted effort. Image/study cache functionality should also be explored for low bandwidth situations.
Allen Scales, vice president, corporate strategy, Emageon, Birmingham, AL
1. [Enterprise Master Patient Index] Integration: Ability to cross-reference patient files between the hospital and clinic for a unified patient record.
2. Web-Enabled: Thin client downloads for easy upgrades and maintenance. Avoid stand-alone viewstations.
3. Web-Enabled Tech QC: Cost effective, robust tools. Avoid standalone tech QC viewstations.
4. Fast Native Advanced Visualization: Easy to use, cost-effective 3D tools for multi-slice CT.
5. IHE (Integrating the Healthcare Enterprise) Conformance: Using standards reduces the cost and headaches of integration now and migration in the future.
Steve Deaton, product manager, Viztek Inc., Jacksonville, FL
All PACS systems that the buyer should be considering are likely similar in regards to toolset capabilities.
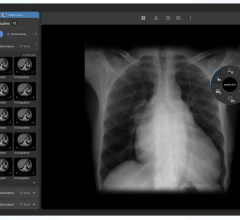
1. One critical issue to keep in mind is ‘ease of use’ because it will affect overall site acceptance of a new product. The PACS selected should closely resemble normal Web-surfing. Viztek’s Opal-RAD PACS offers simple searching, single click-to-action, and native Internet Explorer functionality. These are all things that should be considered. A worklist, which is natively embedded into a Web page, can be easily deployed and supported.
2. Installation of the software client should follow suit. The client should install without any need for license keys or software dongles. Licenses should be verified against the server, and allow users to deploy client viewers wherever they please. Needs will change down the road, so users should not have to plan on scheduled installation times with the PACS vendor or administrator.
3. I would advise the potential buyer to look closely at their workflow. Most PACS offer similar tools, so it is time for systems to encompass more than viewing. Viztek’s Opal-RAD PACS has added features such as dictation/transcription integration will improve workflow and save radiologists’ time. Integrating the dictation/transcription process into the PACS brings increased accountability for reading times. Radiologists should not have to toggle between different applications to dictate, approve reports and lookup previous reports.
4. Remote viewing capabilities should be considered when purchasing PACS today. High-speed Internet access is available in most locations, and radiologists now have the freedom to read outside the imaging facility. The PACS purchased should allow more than simple access to images remotely. Opal-RAD provides the radiologist with options to improve opening times of images. Manual prefetch is one way to allow users to pull exams to a local PC for faster viewing. More appealing than the manual prefetch is the theory of automated pulling mechanisms. Viztek’s OnCall feature allows users to login from any PC and turn it into a secure auto-route recipient of the PACS. With one simple mouse click, all new cases will flow to the radiologist’s computer immediately. The list updates live, and new cases continue to be automatically routed to the radiologist’s PC, without the need for manual intervention.
5. Viztek’s PACS uses industry leading backend components. Previous trends to use proprietary systems such as Linux and Unix have proven to be costly to support. PACS should run on platforms which are more widely deployed and can be more easily supported. Microsoft .NET framework and SQL databases are examples of standards which have proved to be robust, capable, and reliable.
Rik Primo, director of marketing and strategic relationships, Image and Knowledge Management division, Siemens Medical Solutions, Malvern, PA
When an outpatient care facility decides to deploy PACS it is often initiated by drastic changes in their environment. The following are some drivers of PACS adoption:
• The newly acquired multi-slice CT is no longer producing just 150 images per patient, but rather 1,500 images per exam.
• Digital mammography now requires the use of specific softcopy viewing tools to explore the wealth of data buried in these digital images.
• Competing diagnostic imaging centers are offering PACS in the same market. Many referring physicians now prefer receiving Web-based images and reports, rather than waiting several days for the report and film folders.
• Referring orthopods want to obtain digital images for use with their new software-based endoprothesis planning tools.
• Outpatient care facilities may contract with a tertiary care hospital. Because of this, many radiologists and referring specialties in the hospital also would like view the images acquired at the outpatient care facility in their PACS.
In essence, environmental changes are the main drivers for PACS adoption. Environments consist of people, processes and products. PACS initiatives must take all of these into consideration in order to be successful. A holistic approach is also required and the first thing to consider when purchasing a PACS system is the needs of the user.
1. People: The PACS user is not only the radiologist, but also the customer of the radiologist, namely the referring physician. One must understand their needs and expectations in order to select the appropriate PACS. Different users also require different tools. Some important questions to ask include:
• Is the PACS capable of providing the required tools?
• Are these tools available from a single workstation?
• Are these tools clinically focused, context sensitive and role-based?
• Will the users also require access to EMRs, lab results, etc.?
• What is the expectation of image and report delivery? Do they all have access to the Web, or will CD distribution also be necessary?
2. Processes: A PACS is not an island in the ocean of radiology. It is merely a tool in the total radiology workflow to view and analyze examinations as well as to diagnose, document and archive image information for many years (depending on state legislation). The processes related to PACS are instrumental in assuring the most efficient and cost-effective patient care.
3. RIS, scheduling processes: PACS workflow should be driven by the RIS which provides the demographics to the PACS, as well as to the modalities. RIS can alert the PACS to obtain prior images of a patient in advance so they may be ready for comparative viewing by the radiologist when the new exam is complete and on the workstation. Finally, the RIS will trigger the distribution of images and reports after signoff by the radiologist. This workflow will require a revisit to the RIS functionality itself. Before PACS, the RIS was mainly limited to radiology administration functions.
Some outpatient care facilities do not have a RIS today, although PACS will require it in the near future. Because of this, an integrated decision should be considered. The RIS should be able to drive the radiology PACS workflow and the PACS should be able to be RIS-driven. RIS should also be able to be driven by the scheduling system. This means that the scheduling system should also be revisited and the complete process of scheduling, exam acquisition, PACS viewing, report and image distribution, archiving and billing should be re-engineered to provide optimal workflow through streamlined processes.
4. Image and report distribution processes: PACS can improve the image and report availability and image distribution performance significantly. The PACS should also be able to distribute images and reports via the Web. This will improve the level of service provided to the referring specialties, and will differentiate the outpatient care facility from the competitors. By enabling radiologists and referring physicians to interact collaboratively, an organization can further improve its service offerings.
5. Product: DICOM is required to enable communication between the outpatient care facility PACS, modalities of different vendors and PACS in other ‘customer’ hospitals. Some important questions to ask include:
• Does the PACS have all the tools required by the users, radiologists and referring physicians?
• Are these tools clinically focused, role-based and context sensitive?
• How easy is it to use these tools?
• Do they have all the same [user interface], and can they run from the same workstation, or do they require separate workstations?
• Does the number of workstations depend on site license, or does one need to purchase an extra license for an extra workstation?
• Can the PACS be scaled up to handle future increases in data volume and number of procedures per year?
• How fast can the PACS display huge studies such as multi-slice CT and digital mammograms?
• How will your PACS handle the backup of the database and images?
• Do you have the staff to manage this? If not, you should consider an off-site ASP service for storage and archiving.
In summation:
• Know your users and identify their needs.
• Revisit the processes: scheduling, exam acquisition, PACS viewing, report and image distribution, archiving and billing.
• Determine if the PACS can be seamlessly integrated in this re-engineered digital workflow.
• Choose a PACS with the right performance and tools, depending on the expectations of the users.
• Choose a PACS that can be easily upgraded to handle continually growing data sets and procedure volume.
• Choose a PACS that conforms to standards , such as HL7 and DICOM, and can implement the Integration Profiles described by IHE (the ability to interface with EMR, portals and other clinical IT systems located in outside hospitals can provide additional benefits).
• Choose a PACS that can interface with an [application service provider]-based remote archiving service to provide redundancy in storage and disaster recovery in the event you can't afford to build and maintain your own infrastructure and backup operations.
• Choose a PACS that can run on [commercial off-the-shelf] hardware and is Web-enabled.
Ulf Andersson, general manager, Healthcare Information Solutions, Carestream Health Inc., Rochester, NY
1. Integration is a key capability. Selecting a PACS that offers easy integration with an existing RIS and other information management systems is critical to achieving an efficient workflow by providing worklist management and reducing the need for manual data entry. Our KODAK CARESTREAM PACS platform is recognized for its ability to be integrated with most modern RIS systems. We also offer integration services that can assist imaging centers with limited IT resources.
2. A fully-featured Web component is critical. Imaging centers need a fully featured Web component that enables fast and convenient access to the radiology report (with key images if needed) and the imaging study. The ability to deliver time-saving dynamic streaming technology to referring physicians and specialists in remote locations is also extremely attractive.
3. Since the shortage of radiologists is expected to continue, imaging centers are wise to employ a PACS that offers full functionality from remote locations. A few PACS platforms enable remote radiologists to use image display and adjustment tools as well as integrated applications (including native 3D, voice recognition, image fusion and others). This equips imaging centers with the flexibility to use remote radiologists for primary or after-hours reading and ensure responsive service for referring physicians and patients.
4. Redesigning workflow can be as important as implementing digital technology. Many hospitals and imaging centers that have installed PACS have not achieved anticipated productivity gains. CARESTREAM Business Diagnostics is a workflow optimization and redesign methodology that streamlines the image management process and eliminates the continued use of inefficient paper-based processes in the new digital workflow. This service, which is based on innovative process improvements used successfully to streamline manufacturing efforts, is available for users of any vendor’s PACS system.
5. Consider an integrated RIS/PACS solution for imaging centers. Facilities that are currently working with outdated RIS and/or PACS solutions should examine the benefits of implementing an integrated RIS/PACS solution designed specifically for imaging centers. The new CARESTREAM Outpatient Solution incorporates a fully-featured RIS with a high-performance PACS and onsite or remote archiving. This platform provides a complete digital workflow including: Exam scheduling and capture, diagnosis with advanced diagnostic tools, digital dictation, transcription, Web-based viewing of radiology reports and key images, billing, claims processing and results distribution. This solution is both scalable and cost effective.
Lenny J. Reznik, director, Radiology IT Americas, Agfa HealthCare, Ridgefield Park, NJ
1. Large Volume Data Set Management. The advent of multi-slice modalities creates unique workflow challenges for the radiologist. Agfa HealthCare is developing more tools that help radiologists handle large volume data sets, consistent with our work with the SIIM TRIP initiative, blurring the lines between different applications such as PACS, RIS, advanced visualization and reporting. Outpatient care facilities should look for a vendor that can minimize the workflow challenges created by multi-slice-modalities.
2. Standards. The best way to protect your investment is to choose solutions that adhere to standards such as DICOM, HL7 and initiatives that use those standards such as IHE, Integrating the Healthcare Enterprise. PACS is a complex radiology IT solution that must work with many other applications in order to produce the productivity your facility needs. Choosing companies, like Agfa HealthCare, that have leadership positions on these standards boards means your PACS system won’t be obsolete in two years because it can’t work with a new modality or IT system.
3. DICOM Archive. Any healthcare facility that has decided to change their PACS vendor can attest to how complex and costly it can be to migrate PACS data. A pure, vendor-neutral PACS archive, like Agfa’s IMPAX Data Center, is a standards-based solution that will assure they won’t have to move their data again and be able to provide all relevant radiology, cardiology and IT Infrastructure IHE profiles, including XDS, XDS-I and PIX that will allow them to easily share information with other facilities.
4. Clinical applications. When looking for PACS, you want flexibility in choosing advanced clinical applications. Tools such as MIP (Maximum Intensity Projection) and MPR (Multi-Planar Reformatting) should be standard on all your display stations, and even if you don’t think today that you will need them, more advanced tools such as 3-D volume rendering ought to be available from the vendor. PACS is a long-term investment and new modalities and newer ways of reading studies make the availability of advanced clinical applications key to success. Agfa HealthCare makes sure a number of choices in clinical applications are available and are harmonized as part of the reporting workflow.
5. Critical Test Results Management. One focus point for Agfa HealthCare’s radiology IT solutions has been addressing radiology’s goal in improved patient safety and improved ability to meet Joint Commission accreditation. The highlights of these goals led to the successful introduction of IMPAX Veriphy Critical Results. IMPAX Veriphy Critical Results solves a universally manual and haphazard process: the phone-based communication of critical test results. Agfa’s solution provides a methodology and audit trail for managing critical result notification.
Tim Kulbago, senior vice president, Strategic Business Initiatives, Merge Healthcare, Milwaukee
The use of PACS to transition from film to digital has occurred across numerous imaging organizations. Solutions have evolved rapidly in the past decade and go far beyond basic functionality to enable the move to filmless. Whether choosing a PACS solution to replace an older system, or to add PACS for the first time, organizations must evaluate a range of ‘next generation’ concepts. These include:
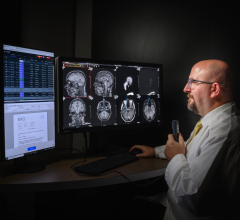
1. Ability of the PACS to reduce ‘down-time.’ Radiologists must move through their reading stack efficiently. They should spend little time identifying and prioritizing cases, searching for patient information, and moving between applications for various tasks. The ‘ideal’ PACS workstation graphically designates the status of a study so that worklists can be filtered in numerous ways (to efficiently divide cases among subspecialists, for example) and so that high-priority cases stand out. The ideal PACS should be configurable for individual radiologists to specify reading preferences. And, with ‘smart’ technology, the PACS should actually learn from the radiologists’ reading patterns – and automatically presents images in the order he/she prefers with the tools he/she prefers. Loading can be hastened by a system that automatically decompresses images to the resolution required for display, and dynamically decompresses even further as the radiologist zooms or magnifies the image.
The ideal PACS puts information at the fingertips or the radiologist, much like a film-based file jacket. For example, the PACS should provide immediate, dynamic access to historical studies/reports, and it should interface with the HIS/RIS so a patient’s study is displayed with clinical history, order information, key images, etc. The PACS workstation should also integrate readily with voice or digital dictation (to avoid time spent moving from one environment to another) and with document management (so that scanned-in documents are readily available and viewable in context.)
2. Ability to specify and individualized settings available at any workstation, minimize the impact of interruptions and optimize clinical reading. No two radiologists are alike and, as such, each has unique reading characteristics. Ideally, the PACS will allow each radiologist to tailor viewing protocols according to his or her preference. Additionally, the PACS should allow these settings to follow the radiologist from workstation to workstation – across a single facility, multiple facilities or even for reading from locations outside the organization. As the radiologist reviews a case, he/she will mark images, measure different lesions and structures, compare priors, etc. For large studies, this can take some time.
Yet often, the radiologist is interrupted – perhaps a STAT case needs immediate review, a technologist asks him/her to check a case to determine if additional views are needed or a referring clinician arrives to review their patient’s imaging studies. Some PACS solutions require the radiologist to close a case currently under review in order to immediately address the ‘interruption.’ In some cases all of the work already performed on that case would be lost and work would need to be redone. An ideal PACS overcomes this inefficiency by enabling radiologists to multi-task on more than one (or even two) cases without losing their place or pace.
Specific clinical functionality is also important. One example is triangulation for MRI and dynamic slab MIP. In some PACS environments, the radiologist is required to go back and forth to triangulate structures. This leaves room for errors. Some newer PACS solutions give the radiologist a little crosshair that can be placed in plane on the structure. A single click brings the crosshair into all the other sequences. Working multiple planes makes is faster and can be very useful for figuring out detailed anatomy, pathology and extent of disease.
3. Ability to enable dynamic communication with peers. Interacting with a full spectrum of caregivers is critically important to radiologists, yet getting a colleague in the same room, finding a specialist on the phone or tracking down a referring physician can be challenging. An ‘ideal’ PACS will enable the community of caregivers to have access to critical information and people. These systems should have tools such as instant messaging, voice-over IP, simple Web interfaces and secure email. This is important today, especially in multi-site centers and specialty clinics when a colleague is likely to be across town rather than across the hall. The radiologist should be able to ask the colleague to provide a second opinion by simply sending a link to a specific study along with a brief message. To collaborate quickly and reduce system load, the PACS should also allow the radiologist to capture and share a key image (a subset of the full image.)
4. Ability to simultaneously load, view and compare larger volumes of images. Newer studies, such as multi-slice CT, breast MR, and PET/CT yield thousands of images and place high demand on a computer’s physical and virtual memory, especially during comparison viewing when current studies are displayed along with the priors. Most solutions are 32-bit systems, which are incapable of loading large image sets completely into memory for display.
Some solutions provide proprietary ‘workarounds’ to address these issues. Yet in many organizations, systems can run slowly or may even stop. Radiologist workflow is interrupted, causing frustration and costly delays, and potentially impacting clinical capabilities. Today’s newest PACS approach leverages native 64-bit processing to overcome memory limitations and system performance issues associated with 32-bit technology. The radiologist can load any study along with as many relevant priors as needed without limitation on the workstation – leading to more efficient and effective reading.
5. Ability to go beyond basic HL7 interfacing and truly integrate the PACS and RIS. As radiology evolves into an information-intensive environment, so too must the PACS evolve beyond the boundaries of conventional capabilities. New PACS solutions are expanding their information models to take in diverse types of information and adding new functionality for more advanced access to this information. HL7 interfacing is no longer enough. New boundary-breaking solutions must focus on providing a single business and clinical application that delivers operational efficiency across the entire organization and a uniquely optimized workspace for radiologists.
Today, some organizations have an extremely strong RIS infrastructure and therefore, have solid information management success, yet their PACS environment is weak. Others have exceptional PACS-enabled image management capabilities, while their RIS lacks important functionality. The resulting asymmetrical environment can create challenges that draw focus away from the organization’s ability to minimize inefficiencies and maximize productivity to sustain or grow a business. This really is no longer about the PACS or the RIS. An organization that simply has the ability to pull images into its RIS will not survive over time. Alternatively, expanding the PACS with richer information models can never address the full picture. In fact, the days of having separate RIS and PACS systems will soon be over.
To get to a really world class system that optimizes the synergies of RIS and PACS functionality, many organizations have found it valuable to start with world class technologies in both the RIS and PACS spaces, such as the solutions available from Merge Healthcare.
This trend of imaging and information coming together into a unified system will continue to unfold as organizations push new boundaries with technology. And, we will see it intensify as advanced clinical applications are developed. It will no longer be good enough to say, ‘here’s our virtual colonoscopy, lung detection or calcium workstation.’ Over time, these systems will be fully integrated into a single information and imaging infrastructure. In this scenario, advanced algorithms can make prior images immediately available for comparison, and software can track and automatically highlight potential problems for the radiologist.
For more information:
www.agfahealthcare.com
www.americanrad.com
www.carestreamhealth.com
www.emageon.com
www.merge.com
www.medical.siements.com/us
www.viztek.net




 November 29, 2025
November 29, 2025