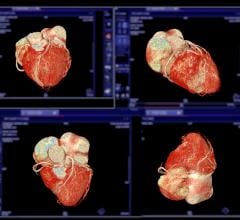
3-D volume rendering showing mid-LAD stenosis. Photo courtesy of TeraRecon Inc.
Although it’s relatively new to coronary artery disease (CAD) detection, computed tomography angiography (CTA) is already facing some competition. New studies are pointing to magnetic resonance angiography (MRA) as equally effective in doing the same thing, without exposing patients to ionizing radiation.
For example, in the February issue of Radiology researchers took 80 patients suspected of arterial occlusive disease and compared the performance of MRA to digital subtraction angiography (DSA) and CTA. DSA is the current standard for this type of evaluation, but in 2.5 percent of cases the procedure causes mini-strokes and, in rare instances, permanent neurological damage.
Kambiz Nael, M.D., research fellow and radiology resident at the David Geffen School of Medicine at UCLA in Los Angeles said the results of the study were comparable to both techniques.
“In the absence of contraindications to MRI, I would recommend MR angiography over DSA and CTA for routine use...,” he said.
So in light of the reduced exposure to radiation, is CTA losing ground in the world of CAD detection?
A Complementary Role
Norbert Wilke, M.D, doesn’t think so. The associate professor of Radiology and Medicine at the University of Florida-Jacksonville says the two modalities are playing an increasingly important and complementary role in the assessment of patients with chest pain.
“CT is a very useful tool in the initial ruling out of significant CAD, which is done in about 70 to 80 percent of cases admitted for chest pain,” he said. “It is a very useful test.”
Advances in multidetector CT have allowed for acquisition of motion-free sub-millimeter resolution images of the heart and coronary arteries with ECG gating in one breath hold, Dr. Wilke said. Because of this and its short acquisition time, CTA holds an advantage over MRA in coronary imaging.
“However, in cardiac CT, there’s going to be around 20 to 30 percent of patients where it’s not that clear cut — whether there’s disease or not and whether the disease is significant or not,” Dr. Wilke said.
It’s in this type of testing that MRA would be very complementary to CTA, he said. It’s also much more accurate than nuclear medicine — early subendocardial perfusion defects can be detected by MR rest-stress perfusion imaging, something often missed by nuclear imaging.
Although CT’s radiation dosages will be further reduced with the newer generations of CT scanners, Dr. Wilke says overuse of CT imaging will always be potentially cancer inducing.
“My personal view is that cardiac CT should not be done in conjunction with another radiating test, such as perfusion nuclear imaging, because it adds another substantial amount of radiation dosage,” he said.
Currently, three separate tests are used to get the same information cardiac MR imaging obtains, Dr. Wilke said: echocardiography, rest-stress nuclear imaging and PET imaging. He said the main reason why MRA should only be used as a secondary tool after an initial CTA screening has to do with time, expertise and money.
“The availability of cardiac MRI is more limited compared to multidetector CT due to higher level of required expertise and preparation and examination time,” he said.
The machine itself can be very costly as well.
“MR imaging is harder to learn, harder to use and is expensive,” Dr. Wilke said. “The upfront investment is quite high, and that’s why people are still retreating to what they’re used to.” He said this includes echocardiography and diagnostic X-ray coronary angiograms — the current standards for functional assessment of CAD.
However, Dr. Wilke believes that using a combination of CT and MR in CAD detection will save hospitals “a huge amount of costs” in the long run.
“Screening with CT can rule out CAD very quickly,” he said. “The majority of people admitted nowadays to the hospital eventually get ruled out, but only after they accumulate costs at the hospital that weren’t necessary in the first place.”


 November 13, 2025
November 13, 2025