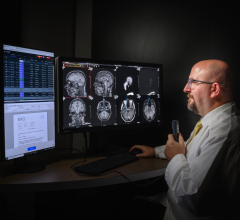
An EHR provides access to clinical information at one time from one place.
Long before U.S. President George W. Bush emphasized the importance of the electronic health record (EHR), cancer treatment centers understood the value of accessing patient information anytime and anywhere.
As radiation oncology becomes more dependent upon images to further guide advanced therapies like Intensity-Modulated Radiation Therapy (IMRT), complex treatment plans are modified or updated as patient response to treatment is gauged, and an enterprise-wide EHR provides immediate access to those updates that are so critical to quality patient care.
Positive Impact on Patient Care
As with most information technology solutions, enhanced patient care is an immediate benefit of direct access to patient data and images. Armed with up-to-date information, physicians can make better patient care decisions. “When physicians are on call, they can immediately access the record from almost any PC on the Edward campus,” said Katherine Lee, a clinical systems specialist at the Edward Cancer Center, part of Edward Hospital, Naperville, IL, who was involved with the implementation of Varian Medical Systems’ VARiS Vision Oncology Information System.
After going live in December of 2004, Lee said that “accessing the patient record from any PC in the center” is by far the biggest advantage, eliminating the need for a file clerk to transport several paper charts. According to Lee, the ability to answer questions for patients on the telephone and to track patient medications has also positively impacted patient care.
Prior to the implementation of IMPAC’s eChart for Radiation Oncology at Alexian Brothers, it was not uncommon for staff to spend valuable time hunting down a patient’s chart. Access to the electronic chart has enhanced to the center’s ability to provide more efficient patient care. “After the implementation, we now start a patient’s treatment one to two days earlier,” noted Karen Stinespring, technical manager and lead therapist at The Cancer Institute at Alexian Brothers Hospital Network, Elk Grove Village, IL. “The paper environment just took longer.” Stinespring also reports that patients are reassured knowing their caregiver has accurate and timely information about their treatment. Data is recorded and verified in the IMPAC eChart, which Stinespring said, “acts like another therapist and prevents any treatment” if information is missing or deemed inaccurate.
“The main issue with an electronic record is that the chart is always available,” said Christy Kesserling, M.D., radiation oncologist at Alexian Brothers. “With an electronic record, we have better checks and balances [throughout the treatment cycle] because all the information is available at once for all caregivers.”
Dr. Kesserling has also seen a positive impact on patient care and greater collaboration between radiation oncology and medical oncology after the EHR implementation. “As a doctor, I can provide immediate answers to questions by medical oncologists, even if the patient is not mine, because the information is readily available at any given time.”
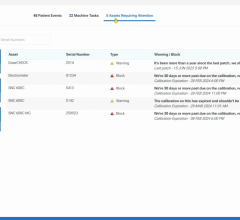
Beyond this, process improvement at Alexian Brothers has leaped forward in Kesserling’s opinion. “Quality assurance is extremely important. We now have an electronic quality checklist that tracks documents, notifies other users of a patient’s status and availability and handles basic housekeeping duties such as charges and consent forms.” The system helps the physician follow-up on test results by assigning a due date when the order is first placed.
Ken Ewers, director of Cancer Center Technology for Diagnostic Imaging and Radiation Therapy Clinical Solutions at U.S. Oncology, noted that “[a]nything we can do to automate the process frees up the clinical staff at our affiliated practices to focus on providing patient care.” Ewers explained that in many practices, the physician or other staff members will use three or four computers, and often, different systems, for different pieces of information. “Our goal is to bring that information together and to enable access to most, if not all, information needed at one time and in one place.” U.S Oncology is currently implementing an EHR to network practices that have expressed interest.
Streamlining Business Models
In addition to capturing patient data, most oncology EMR systems also provide electronic charge capture for billing, and Edward Cancer Center is currently migrating to this feature. “We’ll be more accurate with billing since charges are based on charting,” explained Lee. “Any time you can remove the human error [factor], you end up with better results.”
Creating a more efficient and effective business model is critical for all healthcare facility administrators, regardless of specialty. For Stinespring, the creation of an electronic quality checklist has enabled her to better manage the department. “I can really check accountability throughout the entire patient care process. If something is not completed, I immediately know why based on this checklist.”
The ability to import and export information is critical to efficiency, which further enhances the business operations of a facility. Both Edwards and Alexian Brothers import relevant patient data from the hospital’s information system. Further, data from the treatment planning system is directly exported to the Oncology Information Management System, which is the system that drives the Oncology EHR, leading to greater efficiency and reduced errors. “With the import and export features, we’ve removed those handwritten notes. There is definitely greater room for error with paper-based records,” said Stinespring.
Since U.S. Oncology uses outside radiologists, a critical component for Ewers has been the integration of diagnostic images and reports from Kodak Health Imaging’s Carestream PACS. “Diagnostic imaging helps identify the progress of the disease and facilitates effective treatment planning. By using more advanced imaging [like PET and CT], we have higher quality images that enables the network physicians to provide better treatment while letting us target that internal target.”
The Kodak PACS, through its infrastructure, is supporting Ewers’ efforts to retain not only the diagnostic images, but also the radiation therapy imaging file within one consolidated archive.
Yet, William F. Knight, chairman of Healthsphere Corp., a nonprofit healthcare advocacy organization, has witnessed first hand the bi-directional transfer of information between multiple specialties. He noted the difficulty in oncology is that its objects are unique in healthcare, not only DICOM RT but also proton (Ion) objects that are currently under review by the DICOM workgroup. “Current IT solutions are generally not designed to handle these ‘objects’ and a greater importance should be assigned to them by PACS vendors,” said Knight.
The challenge is to populate this enterprise-wide EHR model electronically from the oncology EMR. “To date, this cannot be done without a sophisticated interface,” Knight added.
Because clinical information has different values based on the lifecycle of that data, Intelligent Lifecycle Management (ILM) technology, such as the one from Acuo Technologies (St. Paul, MN) and Teramedica Healthcare Technologies (Milwaukee, WI) used at MD Anderson in Houston, TX, creates logical pools of information based on user-defined clinical rules. These rules or protocols set by the user can determine where clinical data is stored, for example, if it is stored online RAID or at an offsite MOD. It can determine how long data such as mammograms, pediatric X-rays and chest X-rays must be stored at particular configurable compression rates. It also provides access controls and audit trails to meet privacy/security guidelines.
Silos of information, however, still exist, and solutions must enable information to move freely. Knight added, “If we don’t implement this as an industry-wide initiative, then the government will force it upon us in much the same way as the roll-out of HIPAA.”





 July 11, 2024
July 11, 2024