
E-Z-EM's PROTOCO2L colon insufflator greatly diminishes patient discomfort.
Colon cancer is the second leading cause of cancer death in the U.S., primarily striking individuals 50 and older. Because the disease can be present without any physical symptoms in its initial stages, regular screening — through a fecal-occult blood test every year plus a sigmoidoscopy every five years, or a colonoscopy once every ten years — is advocated for this age group.
Yet, despite the American Cancer Society’s recommendation, an unprecedented 60 percent of the over-50 population fail to have a colonoscopy performed, according to Chicago gastroenterologist Jeffrey H. Goldman, M.D. The reason? For many, it is the procedure’s invasive and delicate nature that makes patients reluctant, causing them to put off the screening test that could potentially save their lives.
Patient-Friendly Alternative
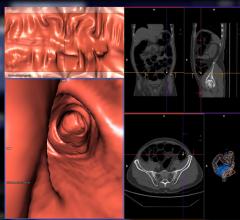
Clinically available for nearly a decade, CT colonography — more commonly known as virtual colonoscopy (VC) — is a patient-friendly alternative to traditional colonoscopy that does not require intravenous sedation and uses CT scanners to image patients in the prone and supine position. This results in cross-sectional views not only of the colon, but also the whole abdomen and pelvis, and the entire procedure can be performed in as little as 15 minutes. The data is then reconstructed in a software package, commonly using a combination of 2-D and 3-D techniques, which provides a “fly-through” representation of the colon that the radiologist uses for final interpretation.
As with traditional colonoscopy, patients must first perform at-home prep work, often considered the most uncomfortable step of any colonoscopy. Fortunately, there are ways to ease patient discomfort and help ensure compliance throughout the VC experience, explains E-Z-EM’s Allyson Mortati, global market manager, virtual colonoscopy. The company’s gentle, easy-to-use LoSo bowel prep is pleasant tasting, while its NutraPrep food kit — the only product of its kind — offers a low residue alternative to the traditional liquid diet. Taken three times a day with meals, the low volume Tagitol V fecal tagging agent marks any stool that may have been left in the bowel.
During the minimally invasive procedure, the colon is distended with either room air or carbon dioxide (CO2) that is inserted through a catheter in the rectum. Room air must leave the body the same way it goes in and for most patients that translates into tremendous discomfort that can last for hours. With E-Z-EM’s PROTOCO2L insufflator, the CO2 is absorbed into the bloodstream and simply expelled through normal respiration.
Deciphering Mixed Messages
The most notable study validating VC’s clinical relevance was performed at the University of Wisconsin School of Medicine and reported in December 2003. Based on the prospective, multicenter trial that involved 1,233 asymptomatic adults, Perry J. Pickhardt, M.D., associate professor of Radiology at the hospital, reported that VC compares favorably with optical, or standard, colonoscopy in terms of the detection of clinically relevant lesions.
Other studies, however, have not been as optimistic. Due to the inconsistency of trial results, and despite its excellent safety record and growing patient acceptance, opinions on VC’s value remain mixed. In addition, the newer and less expensive technique is currently not reimbursable as a screening tool; however, local coverage decisions may be having an impact. In a growing number of states, Medicare does cover VC when it is performed due to incomplete results from a standard colonoscopy.
Moreover, the currently underway American College of Radiology Imaging Network (ACRIN) trial will seek to produce a definitive consensus on VC’s use as a widespread colorectal cancer screening tool. Comprised of nearly 2,300 patients at 15 sites nationwide, it is anticipated that trial results may be instrumental in persuading patients to undergo minimally invasive colon screening.
Is CAD the Answer?
One refinement that has the potential to propel VC into the medical mainstream is computer-aided detection (CAD). CAD serves as a “second read”, helping radiologists — even those accredited in CT and CT colonography — accurately interpret polyps and lesions.
“Everybody thinks they are great and none of us are,” said Steve Halligan, MB, BS, M.D., MRCP, FRCR and professor of Gastrointestinal Radiology, University College London. “We were performing a study where you examine the colonography first without CAD and then you activate the CAD. When I activated the CAD, it showed me a polyp that I had missed,” he admitted.
Dr. Halligan and colleagues have performed a number of similar studies in the last several years. One recent study implemented a cross-over design where readers used one of two different paradigms — the first was CAD with a 2-D display and the other a 3-D display, which outside of the context of CAD, according to Halligan, is believed to be the best way to view CT colonography studies.
“We found that there was no difference between the sensitivity for polyp detection between the two paradigms, but that CAD was faster,” said Dr. Halligan.
The study included 19 patients with 19 polyps one cm or larger. The CAD software (MedicSight’s ColonCAD) correctly identified 17 of those polyps, while on average 10 of the 19 polyps were identified without CAD. What Dr. Halligan and colleagues discovered was that once the readers, who were accredited in CT, but not necessarily in CT colonography, activated the CAD, their findings did not rise from 10 to 17, as one might expect.
“They jumped up by an average of one polyp, which is fascinating,” said Dr. Halligan, “because they were having real polyps correctly prompted to them and they were choosing to ignore them.” This, according to Dr. Halligan, underscores the requirement for proper training on CAD.
“CAD is an adjunct — a very welcome adjunct in my opinion — that helps you improve the cause of your report and works in combination with good training,” said Halligan. Even with CAD, “[radiologists] still need hard training and accreditation and audit to keep their performance at a high level,” he stressed.
Based on many years of research, The University of Chicago has also developed an effective and sophisticated colon CAD technology, which they have licensed to R2 Technology (recently acquired by Hologic Inc.). The investigational software is being integrated into R2’s ImageChecker CT CAD system, a system that has already proven itself in mammography applications. The VC CAD product is expected to enter the market within a year.
Opponents to VC point out that even with CAD, the newer technique is not a replacement for standard colonography because if a polyp is found, the conventional test must still be performed to remove it. On the other hand, if a polyp is identified through VC, some facilities are equipped to simply wheel the patient down the hall, administer sedation and remove the lesion; the patient does not need to reschedule the additional procedure or endure another bowel prep. As Dr. Goldman reminds his patients, 50 percent of all colonoscopies [virtual or standard] are negative, meaning no immediate further action is needed.


 February 06, 2024
February 06, 2024 









