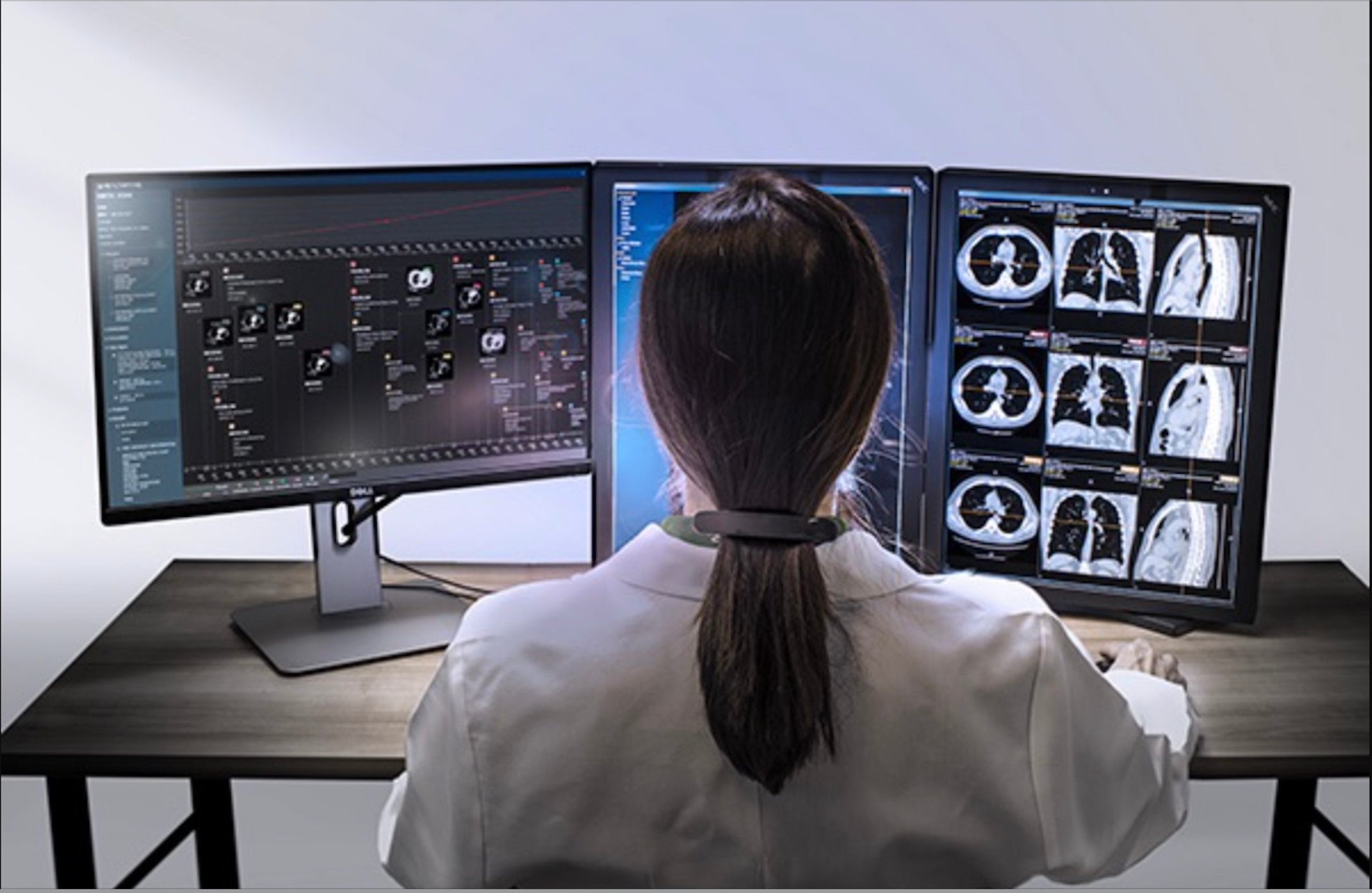
Image courtesy of HealthMyne
The promise of personalized medicine, with its potential for treatments tailored to individual patients’ genomic footprints to generate better outcomes, has long tantalized the life sciences industry.
Now, advanced imaging analytics and the extraction of high-dimensional data from medical images, called radiomics, is emerging as the other side of the personalization coin. By adding an individual patients’ tumor phenotypic (structural) information coupled with the patients’ genetic data, drug developers can create more precise therapies.
Radiomics enables life sciences companies to conduct clinical trials with greater accuracy and speed by leveraging insights about the characteristics of lesions and tumors that are not discernible from traditional reading methods of standard imaging modalities such as computed tomography (CT), magnetic resonance imaging (MRI) or positron emission tomography (PET) scans.
For drug developers, radiomics can contribute value in delivering the last mile in personalized medicine. The combination of genomic data, plus the type of phenotypic data radiomics derives from images, provides even greater adaptability to clinical trial design by mapping the effectiveness of drugs, showing whether treatments under trial are more effective for patients with shared characteristics.
The Basics of Radiomics
Traditionally, when radiologists review images of lesions or tumors, the view has been limited to just two dimensions — long and short axis. Accordingly, clinicians’ primary method of evaluating lesions’ progress has been measuring with digital calipers the vertical and horizontal axes to determine any changes to the lesion. That leaves a lot of key information out of the equation.
In reality, lesions and tumors have multiple dimensions, along with a myriad of other structural characteristics that define them. Human cancers in particular exhibit strong phenotypic differences that can be visualized noninvasively by quantitative or radiomics enhanced medical imaging.
By using artificial intelligence (AI) to discern and compute data from medical images, radiomics enables drug developers to profile a patient, tumor, and therapy across multiple dimensions to find patterns and similarities that would otherwise be unobtainable.
Greater Personalization of Trials
The introduction of adaptive clinical trials has resulted in reviews and analyses being performed throughout the process. For example, if relevant data from laboratory work, imaging or other sources presents itself, the trial can be adapted — with regulatory approval — to account for these factors. The more data that is captured and analyzed as the clinical trial proceeds, the more precise and accurate the conclusions the trial will yield.
Radiomic data is a positive addition to this dataset. By showing previously hidden data and patterns within a lesion, this data can be an early indicator of the effectiveness of the treatment. Linking tumor phenotype and mechanism of action of a novel drug helps address tumor aggressiveness, metastatic potential and tumor response to therapy.
On a broader scale, radiomic data can accelerate or shorten adaptive clinical trials by delivering greater focus. For example, if radiomic data reveals early in a trial the shared patient characteristic for which a therapy is most effective, researchers can concentrate their efforts on those patients. Life sciences organizations can also determine if the market for a particular drug that appears to benefit only a small subsegment of the target population is significant enough to continue pursuing.
Delivering Better Phase 3 Outcomes
The transition of clinical trial for Phase 2 to Phase 3 marks one of the steps along the drug development journey where the greatest risk of wasted time and investment lies. However, researchers can leverage radiomics to gain a greater understanding of the characteristics shared by those for whom the treatment has been most effective, and those for whom it has had little to no effect.
They can then recruit patients who share the targeted characteristics to see if there are even deeper similarities, or if there are any barriers within what appears to be the target group that would prevent success. With this greater focus, life sciences organizations can shave a significant amount of time off a 10-year trial process, substantially reducing costs while bringing the most optimal treatments to every patient every time.
Data that Justifies Costs to Health Plans
While the benefits of personalized medicine are mostly focused on health outcomes, the data generated by radiomics are also valuable. It can be used in justifying the cost of a particular therapy — especially one that costs appreciably more than a competitive product — to health plans.
Imaging biomarkers generated through radiomics add to the clinical evidence supporting the effectiveness of a particular therapy. Rather than being a “one-size-fits-all (sort-of)” approach, data acquired through radiomics enables life sciences organizations to quantify how much more effective their new product is for a set or subset of patients with a given condition.
This apples-to-apples comparison can be linked to economic projections to show why a larger investment now will pay greater dividends over the lifetime of a member, framing the discussion in terms of value-based care. Life sciences organizations may also be able to demonstrate that the faster and more certain improvements generated by the new therapy are likely to shorten the amount of time spent in treatment, reducing the overall cost of care.
Although the life sciences industry has made great progress in its pursuit of fulfilling personalized medicine’s promise, there is no question that work remains to be done. Radiomics represents the missing link that adds individualized patients’ phenotypic data to their genomic information, enabling drug developers to advance more targeted, precise therapies.
Rose Higgins serves as chief executive officer of HealthMyne, a pioneer in applied radiomics, which is the cutting-edge field of extracting novel data and biomarkers from medical images.




 August 06, 2024
August 06, 2024 








