Image courtesy of GE Healthcare
Burnout in the medical profession is not uncommon, particularly as clinicians have become more overwhelmed by growing patient loads, regulatory requirements, and the implementation of new systems and processes that change the way they practice medicine. Now more than ever, this exhaustion has become overwhelming in the radiology field.
According to a recent report by Medscape, the rate of radiologist burnout has grown substantially. In 2017, radiology ranked 20th in the medical specialties reporting burnout. In 2018, it increased and is now the 7th highest, ranking just below high-pressure fields like critical care, obstetrics/gynecology and emergency medicine. Moreover, the survey noted that 45 percent of radiologists reported feeling burnt out, compared with 42 percent of the overall physician population.
There are several factors contributing to this in the medical field. These include too many bureaucratic tasks; spending too many hours at work; becoming accustomed to increasing computerization at work; insufficient compensation; decreasing reimbursements; as well as increased emphasis on profit over patients.
The Role of 3-D Mammography in Burnout
In addition, radiologists face some specific industry factors and stressors of their own, such as changes in medical imaging technology. Consider the move from 2-D mammography to digital breast tomosynthesis (DBT), also known as 3-D mammography. In the last two years, the number of DBT systems in use at certified mammography facilities in the U.S. has grown rapidly, according to the U.S. Food and Drug Administration (FDA). From June 2016 to Dec. 1, 2017, the number of DBT machines in use grew from approximately 3,300 machines at 2,400 facilities, to 5,400 systems at 3,800 facilities.
Unlike traditional 2-D mammograms, which result in only four images to analyze, DBT produces massive data sets comprised of hundreds of images. This requires radiologists spend significantly more time to review and interpret each breast exam. With more images to review for each patient, radiologists risk missing an important clue to early-stage cancer and have a harder time comparing mammography images from year to year. Considering that breast cancer is one of the most commonly diagnosed, and deadly, cancers in American women — more than 325,000 new cases of invasive and in situ breast cancer were expected to be found this year alone — radiologists feel the pressure to not be wrong, or miss the signs of breast cancer in their patients. This alone adds to their daily stress and overall feelings of fatigue.
Because there is no one panacea for radiologists’ burnout, practices must take several key steps to address this among radiologists.
1. Minimize Administrative Burdens
Since bureaucratic tasks were listed high on the Medscape report’s reasons for burnout, practices should consider hiring an individual — such as a reading room coordinator — to manage phone calls, pull records and help track down doctors for consultations. Having someone dedicated to these tasks will free up radiologists and allow them to focus more deeply on their core job — reading and interpreting images and focusing on providing quality patient care.
2. Set Daily Priorities
Whether its finding the time to interpret the toughest cases, encouraging more peer-to-peer interaction or taking needed breaks, practices should encourage radiologists to set daily priorities and stick with them. For example, some radiologists may often feel so overwhelmed with the number of cases and quantity of images looming over them that they feel as if they cannot take a short break or head out for lunch. Simply encouraging them to build in a half hour each day to get away from their monitors and have lunch or coffee with coworkers can help radiologists gain a fresh perspective and escape the grind.
3. Leverage Cutting-edge Technology to Improve Efficiency
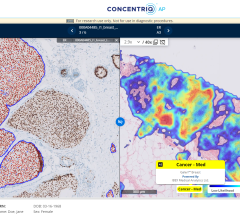
Sure, getting used to new technologies can be a stressor for any medical professional. However, with so many images to read, radiologists can truly benefit from technology that simplifies, not complicates, their processes. This is where artificial intelligence (AI)-powered software can be extremely impactful. Solutions that leverage AI and deep learning are now being used to speed up DBT interpretation time and improve reading workflow. These solutions have become smarter and more adept at identifying cancer as they are trained on breast imaging data, automatically highlighting suspicious areas and enabling radiologists to focus on areas they should review more closely. These detection solutions have shown incredible promise for improving clinical performance for identifying cancer, while reducing radiologist reading time by more than half.
The spike in radiologists who indicate they’re struggling with burnout should be of great concern to the medical industry, as these professionals are on the front lines of patient care. With early cancer detection playing such a crucial role in hastening the path to treatment and improving survival rates, it’s important for the industry as a whole to come together to help reduce radiologist burnout and, most importantly, to help radiologists continue to work toward providing more effective and efficient care.
As Vice President, Medical Director at iCAD, Jeffrey Hoffmeister, M.D., has participated in developing mammographic artificial intelligence (AI) solutions for 25 years. He has provided clinical insight to engineering and marketing teams and managed the design and implementation of clinical studies for FDA approval of mammographic AI products, from iCAD’s first mammography CAD product, SecondLook, in 2002 to iCAD’s PowerLook Tomo Detection and most recent digital breast tomosynthesis AI solution, ProFound AI.



 July 30, 2024
July 30, 2024