A team of California-based breast imagers and breast cancer risk specialists have developed a website to help navigate the new challenges posed by breast density notification laws, according to a special report published online in the journal Radiology.
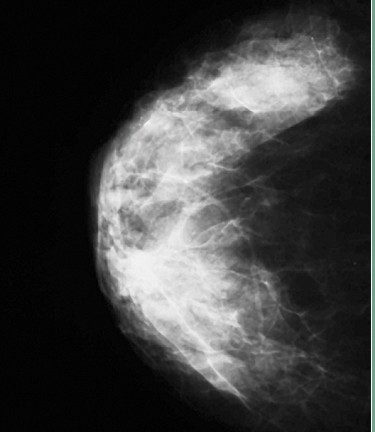
While mammography is considered the best single modality for population-based screening, its sensitivity is diminished by up to 20 percent in patients with dense breasts (breasts with a higher ratio of fibroglandular tissue to fat). This reduction in sensitivity is due for the most part to masking, a phenomenon in which surrounding dense breast tissue obscures a cancer on mammography.
In response, several states have adopted laws requiring patient and referring physician notification when the interpreting radiologist determines that the pattern of fibroglandular tissue on a patient’s mammogram is considered dense.
In California, mandatory reporting requirements took effect on April 1, 2013. The law requires that patients with dense breast tissue on screening mammography receive notification in writing, with advice on discussing their screening options with their primary physician.
“The legislation was prompted by breast cancer advocacy groups motivated to educate women regarding the limitations of mammography,” said Jafi A. Lipson, M.D., assistant professor of radiology at Stanford University School of Medicine in Stanford, Calif.
The California law has potentially enormous implications, as approximately 50 percent of women undergoing screening mammography are classified as having either “heterogeneously dense” or “extremely dense” breasts. For California alone, this could mean two million notification letters a year, and a significant increase in supplementary screening with MRI and ultrasound.
The broad classification of breast density under California law does not take into account the varying risk levels among patients with different breast densities. When risk is expressed relative to average breast density, the risk for the 40 percent of women with heterogeneously dense breasts is about 1.2 times greater than average and the risk for the 10 percent of women with extremely dense breasts is about 2.1times greater than average. Therefore, breast density is a risk factor, but not a strong one.
“While additional screening for women with extremely dense breasts could prove beneficial, supplemental screening of the approximately 40 percent of California women with heterogeneously dense breasts would result in very substantial additional cost to the healthcare system,” Lipson said. “There also is concern that the increased use of supplementary screening will ultimately expose some patients to more harm, in the form of false-positive results, than good.”
To help address these challenges, Lipson and colleagues in the California Breast Density Information Group (CBDIG) created an online document to answer frequently asked questions about the efficacy, benefits and harms of supplementary screening tests.
“Increased patient awareness may be considered a benefit, although there are also potential harms of notification, including awareness without a clear path forward for women and care providers, increased unsubstantiated anxiety, potential for misunderstanding or overestimation of density-associated risk and increased propensity to over-screen,” Lipson said.
CBDIG recommends an individualized risk-based approach for guiding the decision-making process. Women with a high risk of breast cancer, such as those with the BRCA genetic mutation, are more likely to benefit from additional screening with MRI or ultrasound, or with tomosynthesis—a promising supplementary screening technology. For women with intermediate risk, the decision to have a screening MRI should be made on a case-by-case basis using a shared decision-making approach.
The benefits of additional screening are diminished in women who are not high risk, while the potential harms remain the same.
“Studies show a small number of added cancers are found with supplementary screening breast ultrasound,” Lipson said. “However, this is at the price of a large number of benign breast biopsies.”
The CBDIG researchers suggested that women who request supplementary breast screening may be rapidly triaged for assessment based on their individual risk factors.
Insurance coverage is likely to have a major impact on supplementary breast imaging. The California legislature did not mandate insurance coverage for any supplementary breast cancer screening tests, and there are no insurance billing codes for screening breast ultrasound or tomosynthesis. Only one state has a notification law and an insurance mandate, so many women who desire certain types of supplementary screening may be asked to pay out of pocket.
The CBDIG document is available online at www.breastdensity.info.


 August 06, 2024
August 06, 2024 








