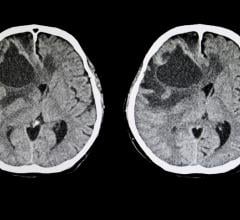
This is an example of a treatment plan with three Hybrid-Arcs within a challenging area of the brain, utilizing arc modulation techniques.
The first applications of and even the term radiosurgery were the idea of Swedish neurosurgeon Lars Leksell, which he published in a seminar article in 1951. Leksell was looking for a minimally invasive way to destroy small tumors and vascular malformations within the skull using radiation. Beams of ionizing radiation do not need a physical opening to enter the skull.
The idea that Leksell devised was to attach a stereotactic frame, a metallic ring, to a patient’s head to help define precisely the position of anything within the skull, like a tumor. This ring would also restrain the head at the time when the machine delivers the radiation treatment beams.
Once the target position is defined, the irradiation would be executed by hundreds of fine radiation beams, each going through a unique path, but all of them aimed at the same target. This allows delivery of a very high dose of ionizing radiation in such a way that in one session you can destroy the tumor you want to treat.
Leksell’s idea was early by many, many years, because in order to perform radiosurgery in the way that we understand it today, we had to wait for development of imaging technology to allow us to define tumors within the brain — like computed tomography (CT), an invention of the 1970s, and magnetic resonance imaging (MRI), which came in the 1980s. In the years 1983 and 1984, radiosurgery really started to become available.
Radiosurgery continued to advance along with the development of microcomputers, and by the end of the 1990s we had a major development — the invention of the micro multileaf collimator (mMLC). Until its introduction, the radiation beams produced by linear accelerators had a circular cross section. To cover irregular tumors, the physician had to divide them into multiple targets that would be filled with “spheres” of radiation. Instead, the mMLC allows us to produce a beam with the same shape of the tumor we are treating, and deliver treatment from any place where the radiation delivery machine sees the skull.
Another Step Forward — No Frames
Another major development of radiosurgery during the last decade is the growing availability of frameless stereotactic radiosurgery, which does not require the use of a metallic ring attached to the patient’s head. We can define precisely the position of the target without the use of a frame and, most importantly, we can deliver the radiation without the frame being applied to the head, just by using real-time imaging at the time of radiation delivery.
This technology demands a much more continuous power to image the patient’s head during the treatment. This kind of equipment requires many additives that are only available when you use dedicated radiosurgery machines.
One of them is Novalis Radiosurgery, developed by Brainlab. The CyberKnife is another system offering real-time image guidance. Since frameless radiosurgery first became available, the number of systems has been growing on both sides of the Atlantic Ocean. Brainlab alone has hundreds of installs.
Significance Now and for the Future
I think the greatest significance of radiosurgery is that it has radically transformed the way we treat brain tumors. On one extreme, tumors that previously were considered incurable, now can be cured or at least controlled for the lifespan of the patient.
For many years, we had to live with tumors at the base of the skull or along blood channels in the skull and treat them with repeat conventional surgeries, because we could not get rid of the whole tumor. But radiosurgery does not have any problem in getting radiation within the structures that are difficult to treat using open surgery. You can bring beams of radiation anywhere within the skull and cure tumors that otherwise could place the patient at high risk of functional damage or even death.
Radiosurgery has had a volume limitation in the past. So it was used mostly for rather small tumors, leaving larger tumors for conventional surgery. But in recent years, the use of fractionated stereotactic radiation has enabled us to treat larger tumors.
The great appeal of stereotactic radiation is that these techniques do not require a physical opening of the head, so you can treat patients as outpatients. The patient can come to the radiosurgery clinic in the morning and go back to his normal life in the evening. The alternative using conventional surgery would require several days in the intensive care unit and additional days in a recovery unit.
Radiosurgery is now being applied more to the whole body, like the lungs, pancreas, liver and other important organs. We believe that in the next decade we are going to see a revolution in the treatment of lung and prostate cancer and liver tumors by treating them as we have done with the skull.
Shaping Cancer Care
Finally, one of the aspects of the radiosurgical revolution is that it has transformed the way we do open surgery. Radiosurgery can be as effective as open surgery in a given setting, but they both have different advantages and limitations. We still use more open surgery for big tumors that place the patient in danger of immediate loss of life or loss of function. Radiosurgery is reserved more for small volume tumors that can be potentially damaging, but are not producing a functional handicap.
Today, these techniques are used in combination. In dealing with difficult tumors, first we can reduce their volume with open surgery, leaving the residual and most difficult part of the tumor to be treated with radiosurgery. We often plan ahead the open surgery to shape the residual tumor so that it can be effectively treated by radiosurgery thereafter. Both techniques are effective, are still needed and are probably going to be needed in combination well into the future.
Roberto Spiegelmann, M.D., is founder and director of the Stereotactic and Functional Neurosurgery and Radiosurgery Unit, The Chaim Sheba Medical Center, Israel, and past president of the International Society for Stereotactic Radiosurgery (ISSR). He presented this information as part of a webinar sponsored by Brainlab during a meeting of the ISSR in Paris in May.


 April 29, 2024
April 29, 2024