September 8, 2010 — A series of studies published in the September Journal of Nuclear Medicine (JNM) show that molecular imaging plays a critical role in the evaluation and treatment planning for a broad spectrum of cancers, including thyroid cancer and lymphoma.
According to researchers, molecular imaging allows physicians to identify the severity and extent of disease and, in turn, provide patients with personalized care. In addition, molecular imaging allows doctors to see how effective a treatment is early in the process, so that changes can be made to ensure the best treatment for each individual patient.
"For patients with thyroid cancer, ‘one size fits all’ no longer applies," said Ravinder Grewal, M.D., corresponding author of "The Effect of Post-therapy 131I- SPECT/CT on Risk Classification and Management of Patients with Differentiated Thyroid Cancer" and an assistant attending physician in nuclear medicine at Memorial Sloan-Kettering Cancer Center in New York. "Through molecular imaging, the paradigm is changing toward more tailored and customized management of treatment. As a result, we can see how far a disease has spread and spare the patient from additional examination, time and radiation exposure."
For the study, researchers performed planar imaging and single-photon emission computed tomography (SPECT)/computed tomography (CT) on 148 patients with thyroid cancer. The results showed that SPECT/CT provided information that reduced the need for additional cross-sectional imaging in 29 patients and redefined the initial risk of recurrence estimates in seven of 109 patients, thereby altering patient management recommendations in terms of frequency and intensity of follow-up studies.
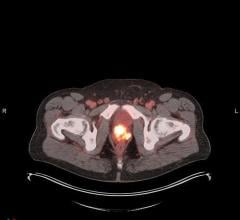
In another study, researchers in Germany used positron emission tomography (PET)/CT with the radiotracer 68Ga-dotatate to evaluate the effectiveness of molecular imaging in monitoring patients with neuroendocrine tumors after undergoing peptide receptor radionuclide treatment. This study evaluated 33 patients at baseline and three months after treatment began. The findings suggest that PET/CT may contribute to the early prediction of treatment outcome in patients with neuroendocrine tumors.
"This molecular imaging technique can help doctors to classify patients according to their prognosis and to choose a personalized follow-up strategy," said Alexander Haug, M.D., corresponding author of the study and a researcher at Ludwig-Maximilians-University, Munich, Germany. "With the use of specific biomarkers, nuclear medicine provides the unique opportunity to perform diagnosis and therapy with the same tracer compound and — with the use of different biomarkers — to provide personalized tissue characterization. Nuclear medicine will be essential for the workup of cancer patients in the near future."
The third study also used molecular imaging to monitor treatment success and aid in planning. Researchers evaluated 104 patients with newly diagnosed Hodgkin lymphoma using fluorodeoxyglucose (FDG) PET after undergoing two cycles of chemotherapy treatment. Of these patients, 93 achieved complete remission after first-line therapy. During a median followup of 36 months, relapse or disease progression was seen in 22 patients. Researchers found that PET is an accurate and independent predictor of event-free survival in Hodgkin lymphoma patients.
"Our findings suggest that early interim FDG-PET may play a pivotal role in Hodgkin lymphoma treatment, tailoring the therapy to an individual level, providing a less toxic treatment for patients with a low risk of failure while attempting treatment intensification for patients regarded as high risk of failure on the basis of the PET findings," said Juliano Cerci, M.D., division of nuclear medicine, Heart Institute (InCor), Medical School of the University of São Paulo, Brazil, and corresponding author of "18F-FDG PET After Two Cycles of ABVD Predicts Event-Free Survival in Early and Advanced Hodgkin Lymphoma."
The fourth study investigated the role of 18F-FDG PET/CT for the early identification of response to therapy in patients with non-small cell lung cancer (NSCLC). Researchers studied 23 NSCLC patients who were treated with a molecular-targeted agent called epidermal growth factor receptor tyrosine kinase inhibitor (EGFR-TKI) and used 18F-FDG PET/CT to monitor the disease before and at one week after administration of EGFR-TKI. Changes in tumor 18F-FDG uptake during treatment were measured by standardized uptake values. Six patients experienced partial response, while 16 patients had stable disease and one patient had progressive disease. The results of the study suggest that early during the course of therapy, 18F-FDG PET/CT can predict response to treatment in patients with NSCLC.
According to researchers, monitoring a patient’s response to treatment can avoid unnecessary toxicity, as well as the cost of ineffective treatment. They also state that the results of the study are promising and consistent with the results of preclinical studies.
Authors of the scientific article, "18F-FDG PET After Two Cycles of ABVD Predicts Event-Free Survival in Early and Advanced Hodgkin Lymphoma," include: Juliano J. Cerci, Felipe A. Pitella, Marisa Izaki, José Soares Junior, José C. Meneghetti, Department of Nuclear Medicine, Heart Institute (InCor), University of São Paulo Medical School, São Paulo, Brazil; Luís F. Pracchia, Camila C.G. Linardi, Valeria Buccheri, Division of Hematology, Clinical Hospital of the University of São Paulo Medical School, São Paulo, Brazil; Dominique Delbeke, Department of Radiology and Radiological Sciences, Vanderbilt University Medical Center, Nashville, Tenn.; and Evelinda Trindade, Health Technology Assessment/Executive Direction, Heart Institute (InCor), University of São Paulo Medical School, São Paulo, Brazil.
Authors of the scientific article, "68Ga-Dotatate PET/CT for the Early Prediction of Response to Somatostatin Receptor–Mediated Radionuclide Therapy in Patients with Well-Differentiated Neuroendocrine Tumors," include: Alexander R. Haug, Björn Wängler, Christopher Uebleis, Paul Cumming, Peter Bartenstein, Reinhold Tiling, and Marcus Hacker, Department of Nuclear Medicine, Ludwig-Maximilians-University, Munich, Germany; Christoph J. Auernhammer, Burkhard Göke, Department of Internal Medicine II, Ludwig-Maximilians-University, Munich, Germany; and Gerwin P. Schmidt, Institute of Clinical Radiology, Ludwig-Maximilians-University, Munich, Germany.
Authors of the scientific article, "The Effect of Post-therapy 131I SPECT/CT on Risk Classification and Management of Patients with Differentiated Thyroid Cancer," include: Ravinder K. Grewal, Joseph Fox, Sunita Borkar, H. William Strauss, Steven M. Larson, and Heiko Schöder, Nuclear Medicine Service, Department of Radiology, Memorial Sloan-Kettering Cancer Center, New York, New York; R. Michael Tuttle, Endocrine Service, Department of Medicine, Memorial Sloan-Kettering Cancer Center, New York, New York; and Joanne F. Chou, Mithat Gonen, Department of Epidemiology and Biostatistics, Memorial Sloan-Kettering Cancer Center, New York, New York.
Authors of the scientific article, "Is 18F-FDG PET/CT Useful for the Early Prediction of Histopathologic Response to Neoadjuvant Erlotinib in Patients with Non–Small Cell Lung Cancer?" include: Tjeerd S. Aukema, Renato A. Valdés Olmos, Department of Nuclear Medicine, Haga Hospital, The Hague, The Netherlands; Ingrid Kappers, Houke M. Klomp, on behalf of the NEL Study Group, Department of Surgery, Haga Hospital, The Hague, The Netherlands; Henk E. Codrington, Department of Pulmonology, Haga Hospital, The Hague, The Netherlands; Harm van Tinteren, Department of Biometrics, The Netherlands Cancer Institute, Antoni van Leeuwenhoek Hospital, Amsterdam, The Netherlands; and Renée van Pel and Department of Pathology, The Netherlands Cancer Institute, Antoni van Leeuwenhoek Hospital, Amsterdam, The Netherlands.
Current and past issues of The Journal of Nuclear Medicine can be found online at http://jnm.snmjournals.org.


 August 09, 2024
August 09, 2024