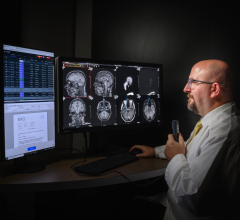
Don Woodlock is vice president and global GM of GE Healthcare Integrated IT Solutions.
The HITECH Act, part of the American Recovery and Reinvestment Act (ARRA), and its impact on radiology is foremost on the minds of everyone in healthcare.
Critical questions surrounding the language of the Act remain unanswered. To gain better insight on the matter, Imaging Technology News spoke with healthcare IT research and development expert Don Woodlock, vice president and global GM of GE Healthcare Integrated IT Solutions.
Imaging Technology News (ITN): Will PACS and RIS qualify for reimbursement under the ARRA?
Don Woodlock (DW): The centerpiece of and the spirit of the HITECH Act is about adoption of general purpose EMR that go across the hospital or physician office EMRs for multi-specialty groups. The definition of meaningful use does mention images; all of the patient’s test results have to be in the EMR, including images and imaging reports. Images need to be part of the electronic health record; [there is] mention of RIS/PACS, but it’s not clearly spelled out that the stimulus will pay for RIS/PACS.
I think the area where we need most clarity is in the outpatient- imaging environment. They are physicians, they see patients, and RIS and PACS is all they have, and they don’t have another electronic medical record in that environment. It’s my feeling that stimulus funds should be provided for physicians [who] use technology even though it isn’t a traditional EMR.
ITN: On June 16th, the definition of “Meaningful use” was released and included reimbursement for imaging described as “multimedia (e.g. X-rays).” A public comment period followed to assist Congress in clarifying this definition. What is the industry doing to represent radiology and convince Congress to include radiology’s needs under the stimulus package?
DW: We are part of several groups that will provide feedback on helping Congress clarify this definition. We are part of Access to Medical Imaging Coalition, which is a group of imaging vendors. I talked to the chair of SIIM, Dr. Erickson from the Mayo Clinic and SIIM was going to get involved in defining meaningful use.
ITN: How will growing volumes of patient data impact radiology?
DW: There will be a big indirect effect on radiology. Radiology has been well automated for many years with RIS and PACS installed over the last decade. But they are basically working with physicians that have not automated at all, and I think the main impact that this Act will have is that there will be EMRs everywhere – hospitals and referring physicians will have EMRs as well. The way radiology interoperates and the workflow of the community will be a lot better when everybody has an EMR.
A couple of examples are the radiologists [who] need the complete patient record to do a good job reading the patient exam. That includes patient history, problems, information about the order; patient allergies will be accessible to the radiologists in the click of the button. The orders will come in, in a cleaner fashion; right now they come in on paper, and radiology can help provide decision support in the ordering process, so that the right test is ordered for the right patient and the report will come in with all of the information that the radiologist needs.
Then, inside radiology they will still use RIS and PACS to read and report on the exam, but then on the way back, the images and the reports will be embedded in the EMR so they will be widely available to every ordering physician that should have access. So the work of the radiologist will be more widely available to physicians that need it and the communication between the radiologists and the rest of the care team will be more effective once everyone is well-automated with IT systems.
ITN: Will the referring physicians be viewing all of the images on the EMR?
DW: That’s right. [For] All the physicians outside of the radiology, their view of the world will be through the EMR. They will go through the EMR to see the full patient record including the imaging tests, the reports and will probably launch a browser to the images. So, we don’t see the EMR becoming a PACS; the images will still be in the PACS, but there will be links to those images and Web browsers embedded in the EMR, so it will be easy for physicians to have access to this information.
ITN: Will the viewer in the EMR also have diagnostic capabilities?
DW: Probably not. In terms of a 6 mega pixel workstation, that will still exist in radiology. But these other physicians will have Web based tools and they may have access to diagnostic workstations and Web viewers, but that’s not really what they are after. They want to see the images, and sometimes use 3D tools, but they are not using it for primary diagnosis.
ITN: Will this impact radiation oncology in a similar fashion?
DW: I think in a very similar fashion. Patients with cancer have a more longitudinal spectrum of care, with multiple visits overtime and multiple physicians involved, and an EMR is a collection point for all these encounters.
ITN: Will there be a return-on-investment (ROI) through these image exchange networks?
DW: Yes, [with the hassle with all these CDs] there are PACS administrators [burning/importing them], productivity drain on the radiologists, [etc]; so there is definitely going to be an ROI for radiology on image exchanges. There is also an ROI for the patients. One of the concerns for the industry is patient dose, especially in pediatric imaging. The best way to reduce dose is to avoid duplicating a test. So if a test has been done in another institution or in the ED or outpatient center, having those tests available helps the patient avoid exposure to that extra dose.
ITN: How will interfacing radiology PACS and EMRs impact radiology workflow?
DW: The workflow will be much more streamlined. So, on the inbound side with the orders and the EMR information, we can eliminate paper with electronic order, we can make sure the physician has ordered the right test according to institution policies, and [they] can see the full patient history without having to log into multiple systems. It all will be assembled together in an EMR. The workflow going out also will be much smoother.
The images will be plugged into the EMR, the reports available on the outbound side. So referring physicians won’t be calling in to get the images or reports, it will be immediately available for all users with the EMR.
The other thing is that there is a JCAHO requirement for critical test results. So the radiologist has to reach out the referring physician in a few hours, depending on the severity. Hopefully when the EMRs are correctly integrated with the PACS, that communication can be really facilitated by IT. You can notify them immediately, it pops up in their EMR, they can acknowledge they have seen this test result and you can track it electronically. So that whole process of phone calls and documentation and post-its will be a lot more automated when EMRs exist.
ITN: Will radiology play a notable role in implementing EMRs?
DW: I think it should [in] a couple of things. The importance of physician leadership and involvement and also making sure there is something in it for the physician. That is one of the reasons PACS got adopted so well; it made radiologists more productive, they have better tools and their workflow is better than in the film environment. And I think EMRs need to have that same focus when rolled out in a hospital or rolled out in a physician group. Radiology has a lot to teach the rest of the organization about healthcare IT.
The other thing is images and radiology reports are a critical piece of the patient record. It’s debatable what percent, but I have heard that 20 percent of a patient record is really the reports and images from radiology. So radiology needs to be involved to plug in that part of the patient record in a logical way into the broader EMR system.
Lastly, the workflow in and out of radiology, the orders, the data coming in, the reports and images going out, and the critical test results communications; that is all workflow between radiology and the EMR. So radiology needs to be very involved to make sure that workflow is designed well, spelled out well, or they may be the victims of a bad implementation.
ITN: Could radiologists teach the rest of the enterprise about interoperability?
DW: Absolutely. Radiology in imaging has been real leaders with great standards like DICOM and HL7. You do not worry about buying an MR or CT from one vendor and a PACS from another vendor and whether they can hook up together – they can hook up together just fine because of a great bed of standards. And collaboration in radiology with IHE and RSNA and other standards groups has been very effective.
ITN: GE Healthcare announced its Stimulus Simplicity program, in which it is offers zero-interest, deferred payment, and bridge loans to qualified buyers who buy and install GE EMR products. How does this relate to GE’s strategy to expand its presence in the fragmented healthcare IT market?
DW: I’ll tell you the problem we are trying to solve with this program. For physicians and hospitals, they really [need] to invest now to get full access to the funding, which starts in 2011. In the current economy, there is a shortage of capital so it is a little [bit] of a problem having the payments come in 2011 and the investments needing to be made now in 2009 and 2010. We wanted to simplify that process, take away some of the uncertainty in the marketplace by offering this finance program. Customers can buy our electronic medical records now, install those, make use of those, get ready for the stimulus funds to kick in, so when stimulus funds do kick-in in 2011, then that is when they have to pay us. So we are trying to align the government stimulus funds coming in the physician groups with the technology investments that physician groups and hospitals need to make.
It is a fragmented marketplace, but we feel confident with our technology and wanted to use the strength of the financial arm of GE to overcome the significant barriers in adoption right now.
ITN: What will be the “meaningful impact” of EMRs on the role of radiologists in the healthcare enterprise?
DW: I think if you have these EMRs in the various locations, you really put the radiologists back on the care team. One of the problems we have had with radiology with this high-level of automation is you can be commoditized at times to just be an imaging reading expert. With more advanced use of EMRs you can become a complete part of the care team, see the full patient record, have the results of your work, like the image and reports available to every physician caring for that patient, and have much better communication and workflow with other physicians involved with the patient. Making a level playing field across healthcare IT really puts the radiologist and the rest of care team on the same page, using the same system and taking care of the patient as a team. So I think it’s really going to be positive for radiology as a profession and allows them to be a better plugged into the care process.
ITN: How does GE Healthcare envision the future of PACS? Will it be an application on a SOA platform?
DW: Absolutely. PACS has been a critical piece of technology over the last 10 years, and as we adopt more healthcare IT in other areas, I think PACS will be even more important. Right now it is mainly designed to run radiology. But the key now, as we have EMRs in these other locations, is to plug that PACS into those EMRs. We can still be great at storing images and displaying images, but we are not solely used in radiology anymore. We [need to plug into the EMRs, make these images accessible, and make the visualization tools accessible for neurologists or orthopedic surgeons or primary care physicians. So PACS becomes a tool for the whole organization instead of just a tool for radiology.
The type of storage and type of tools mean PACS will be somewhat separate from EMRs because the technology is different and what you do with it is different, but they can’t be separate islands. PACS has to be plugged into the EMR world because that is the lens through which all of the other physicians throughout the community will be seeing the patient data.


 July 25, 2024
July 25, 2024