
May 29, 2009 - In the article "CMS's Landmark Decision on CT Colonography — Examining the Relevant Data," by Sanket S. Dhruva, M.D., Steve E. Phurrough, M.D., M.P.A., Marcel E. Salive, M.D., M.P.H., and Rita F. Redberg, M.D., M.Sc., which appeared on nejm.highwire.org on May 27, 2009, the New England Journal of Medicine (NEJM) praised CMS for basing its decision on evidence-based medicine.
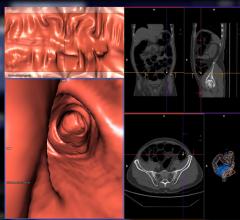
"In an unprecedented endorsement of evidence-based medicine, the Centers for Medicare and Medicaid Services (CMS) recently decided to deny coverage of computed tomographic (CT) colonography for cancer screening, concluding that "the evidence is inadequate."1
The CMS emphasized that the "pivotal, overarching concern" in its decision was the fact that the findings of trials showing a benefit of screening with this method were not necessarily generalizable from the study populations to other groups of patients. In particular, the CMS noted that the mean age of participants in the studies that were cited in support of coverage was significantly lower than that of Medicare beneficiaries. There were no studies evaluating this technology in the elderly, nor were there analyses of subgroups of participants over 65 years of age.
Does the CMS's strict application of evidence-based analysis herald a shift in its approach to national coverage decisions? We hope so.
Although it may seem obvious that a new therapy should be shown to benefit patients in the Medicare population before taxpayers pay for it, in practice such proof has often not been required. In 2007, we surveyed 141 clinical trials that the CMS had used as the basis for six decisions regarding coverage of interventions for cardiovascular disease in the past decade.2 We found an age disparity similar to that cited in the decision regarding CT colonography: the mean age of study participants in the cardiovascular trials was 60.1 years — well below the average age of Medicare beneficiaries. As the CMS found with CT colonography, the trials we reviewed largely did not report outcomes according to age group. These findings suggest that many previously approved interventions may lack evidence of benefit in the Medicare population — the group for which U.S. taxpayers are footing the bill. We believe that the CMS's decision in the CT colonography case, therefore, is a long-overdue step toward meaningful validation of clinical-trial evidence in Medicare beneficiaries.
Our optimism, however, is cautious. Powerful pressure will inevitably be applied to the CMS. Indeed, after the agency published its draft decision in February, proponents of CT colonography, in a now-familiar pattern, quickly mobilized. More than 350 comments were submitted to the CMS by interest groups, many with a financial stake in use of the technology. Radiologist groups and manufacturers of CT equipment, among others, launched a write-in campaign, conducted congressional briefings, and persuaded 56 members of the U.S. House of Representatives to sign letters urging the CMS to reconsider. Advocates for the medical-device industry asserted that the agency lacked the authority to consider data on cost-effectiveness in its decisions. Already at least one representative, Kay Granger (R-TX), has issued a press release expressing the hope that the CMS will reconsider its decision.3
The CMS's handling of CT colonography is a departure from some of its past decisions. Under similar circumstances 2 years ago, the agency issued a draft decision withdrawing broad coverage of cardiac CT on the grounds that there was insufficient evidence of benefit in the Medicare age group. Medicare contractors had reimbursed for the technology under local coverage rulings since the fall of 2006, after the CMS had initially declined to issue a national coverage decision. When the CMS reopened its consideration of cardiac CT and issued a narrower draft decision memo, it received a flood of letters in protest. (Rather absurdly, proponents of cardiac CT argued, among other things, that the CMS had never before insisted on evidence of benefit, and it would be unfair to discriminate against this particular technology by imposing such a requirement.) In the face of these letters and considerable congressional pressure, and thanks to an internal decision that withdrawing coverage required evidence of harm or lack of benefit, the CMS withdrew the more restrictive draft national decision and issued a final decision that maintained generous local coverage.4 Given this history, we worry that the CMS may waver in the face of the struggle between science and politics.
Indeed, it is worth asking why the CMS has acted differently this time. Perhaps the agency is responding to the current economic reality: with the Medicare hospital insurance trust fund projected to become insolvent by 2017,5 the CMS no doubt recognizes the need to ensure that we are spending Medicare dollars, first and foremost, on improving the lives of Medicare beneficiaries. With Medicare expenditures increasing at an unsustainable pace, the CMS appropriately — indeed, necessarily — considered whether the procedure is effective in its beneficiaries.
Regardless of whether we are confronting an economic crisis, a policy of insisting on data relevant to the Medicare population is commendable and has a broader application. We suggest that in future coverage decisions, other subgroup data should also be considered. Our above-mentioned study revealed that 75% of participants in cardiovascular clinical trials are male, whereas men make up only 42% of the Medicare population. Outcome reporting according to sex occurred in only 18% of trials. Given the sex differences in the safety and effectiveness of medical interventions and the fact that most Medicare beneficiaries are women, it is crucial to have data on risks and benefits in women. Furthermore, only 5% of studies reported data on race, and only 1% stratified results according to race.2 In its decision on CT colonography, the CMS noted in particular the lack of data in black patients, who have an increased rate of death from colon cancer.
These disparities indicate that researchers need to carefully consider the epidemiology of the relevant disease and to ensure that studies are adequately powered to provide meaningful data on discrete subgroups. We hope that this decision by the CMS will spur the enrollment of older patients, women, members of racial minorities, and other poorly studied subgroups and the reporting of subgroup data in more published clinical trials.
Another important fact distinguishes the CMS's latest decision: screening for colorectal cancer is one of very few procedures for which the CMS is specifically authorized to consider costs. (The Social Security Act grants such authority for colorectal-cancer screening tests, prostate-cancer screening tests, and certain other preventive services.) In our view, given the economic realities facing Medicare, health care reform must include explicit authority for the CMS to consider costs in all its coverage decisions in order to assess the true value of a given procedure. The agency's examination of value would acknowledge the crucial importance of age-specific data on clinical effectiveness as well as cost-effectiveness in the population for which the CMS is responsible. We applaud this landmark decision, and we hope that the agency remains firm in its evidence-based approach and extends its application as health care reform proceeds.
Dr. Redberg reports serving as a member of the California Technology Assessment Forum. No other potential conflict of interest relevant to this article was reported.
Dr. Redberg served as a member of the Medicare Evidence Development and Coverage Advisory Committee from 2003 through 2006, and Dr. Phurrough was director of the Coverage and Analysis Group at the CMS when the proposed decision on CT colonography was released in February 2009. The opinions expressed in this article are those of the authors and do not necessarily represent the positions of the CMS or the U.S. government.
Source Information
Dr. Dhruva is a resident, and Dr. Redberg a professor of medicine, at the University of California, San Francisco, School of Medicine, San Francisco. Dr. Phurrough is a medical officer at the Agency for Healthcare Research and Quality, Rockville, MD. Dr. Salive is the director of the Division of Medical and Surgical Services at the CMS, Baltimore."
This article (10.1056/NEJMp0904408) was published on May 27, 2009, at NEJM.org.
References:
1. Centers for Medicare and Medicaid Services. Decision memo for screening computed tomography colonography (CTC) for colorectal cancer (CAG-00396N). (Accessed May 26, 2009, at https://www.cms.hhs.gov/mcd/viewdecisionmemo.asp?id=220.)
2. Dhruva SS, Redberg RF. Variations between clinical trial participants and Medicare beneficiaries in evidence used for Medicare national coverage decisions. Arch Intern Med 2008;168:136-140. [Erratum, Arch Intern Med 2008;168:774.] [Free Full Text]
3. Granger K. CMS made wrong decision in prohibiting Medicare reimbursement of virtual colonoscopies. (Accessed May 26, 2009, at http://www.viatronix.com/pdfs/Granger.pdf.)
4. Redberg RF, Walsh J. Pay now, benefits may follow -- the case of cardiac computed tomographic angiography. N Engl J Med 2008;359:2309-2311. [Free Full Text]
5. Pear R. Recession drains social security and Medicare. New York Times. May 12, 2009:A1.
For more information: nejm.highwire.org/cgi/content/full/NEJMp0904408

 February 06, 2024
February 06, 2024 








