
May 8, 2009 - The debate heats up amongst doctors in the advent of the Centers for Medicare & Medicaid Services (CMS) decision on reimbursement for virtual colonoscopy (also known as CT colonography or CTC). CMS will determine whether or not Medicare beneficiaries will have access to virtual colonoscopy, a noninvasive colon cancer screening procedure with the potential to increase low screening rates and save lives.
Medical professionals are taking advantage of the public comment period to let their voices be heard across the CMS Web site (https://www.cms.hhs.gov/mcd/viewpubliccomments.asp). Most comments reflect a strong urging toward reimbursement for virtual colonoscopy, such as the posting from Kyle Kreinbring, M.D., of Advanced Radiology, S.C.
“I am writing to voice my strong disagreement with Medicare’s recent denial of coverage for virtual colonoscopy. We are all aware that colon cancer is a major concern to all American’s age 50 and older, that colon cancer kills more Americans each year than breast cancer and AIDS combined, and that appropriate screening is the only way to prevent colon cancer.
"As radiologists who have reviewed the literature, we are shocked by the conclusion. Large, randomized and blinded studies have been published in well-respected journals. This includes several articles in arguably the most esteemed journal, The New England Journal of
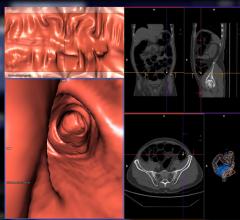
Medicine. Using updated technique and software, the results have been very clear…CTC is a valid, sensitive and safe modality for detection of polyps and cancer. The concerns over radiation and incidental findings seem to be a technique to detract from the real success of CTC. With new protocols and effective dose control the radiation dose is negligible, especially in this population of older patients. In well-trained hands the chance of significant incidental findings is approximately 3%. This is a low price to pay for effectively eliminating the risks and costs associated with screening optical colonoscopy. There has not been a reported perforation or bleed related to CTC. Incidental findings can be managed with the described C-RADS system; a system modeled after the BI-RADS system to classify incidental findings and their significance.
"This technology has the chance to be a life-changing event for many Americans. It will encourage more patients to be screened, which is the ultimate goal,” he said.
Gastroenterologist, Dennis Ahnen, M.D., Denver VA Medical Center and University of Colorado Denver School of Medicine, expresses his disappointment that “to learn of the proposal to not include CT colonography as an acceptable and reimbursable option for colon cancer screening. I think this is a mistake,” he wrote. Dr. Ahnen succinctly weighs the pros and cons of CT colonography versus optical colonography, concluding that these are the reasons why he would endorse Medicare reimbursement for CT colonography.
1. It is now well established that CT colonography, if done by well-trained radiologists with state of the art equipment, is a highly sensitive test for detection of both cancer and significant (>6mm in size) adenomas of the colon; studies have shown that it is as good as optical colonoscopy for detection of these lesions. The concern that CT colonography would be more likely to miss "flat" adenomas is not proven and none of the well done comparative studies have shown that CT colonography has a higher miss rate of any type of polyp (be it flat or not) 6 mm in size or larger. Although CT colonography does not detect diminutive (
2. The concern about variable quality of CT colonography in the community is real but it is equally true or even moreso for colonoscopy. It is well established that colonoscopy quality as measured by cecal entubation rates, withdrawal times, adenoma detection rates and/or complication rates varies widely among endoscopists so that high quality screening is required for both CT colonography and optical colonoscopy.
3. The concern about the cancer risk of radiation exposure with CT colonography is appropriate but theoretical (back-extrapolated from exposure data to much higher doses or radiation) and is much less than the radiation exposure of a barium enema which is covered as a screening option by Medicare.
4. The concern about extraintestinal findings possibly leading to higher costs without better health care is also a legitimate concern, but it is uncertain whether the overall balance of these effects is harmful or beneficial nor what the magnitude of the effect would be in practice. A similar argument is not made for the unintended consequences of other screening tests like false positive fecal occult blood tests that lead to negative colonoscopies, which may be followed, by upper endoscopy and/or capsule endoscopy to look for a source of the blood in the stool. I think that issue of extraintestinal findings could be minimized by guidelines about which lesions should be followed up and which workups Medicare will pay for.
5. The inability to biopsy or remove lesions is a real disadvantage of CT colonography, so it would not be a good choice in a population that would have a high pretest probability of having a polyp seen but there are populations that have a low risk such as those with a negative previous colonoscopy where CT colonography would be a good and cost effective alternative to colonoscopy.
6. CT colonography has some distinct advantages over optical colonoscopy in that it is less expensive, associated with less of a risk of both the procedure and the sedation and is much more convenient for the patient.
Overall, it seems to me, that CT colonography is being held to a higher standard than other screening tests, and I would urge you to reconsider your proposed ruling.
A notably sharp comment by Mark Albright questions the judgment of CMS decision-makers. Albright argues that: “History is replete with examples of governments, politicians, philosophers and businessmen making colossal blunders while clinging to mistaken ideals even in the face of significant evidence to the contrary…Any failure to approve reimbursement of CT Colonography (“CTC”) for colon cancer screening would promptly take its place as among the biggest, costliest and deadliest gaffes in the history of public health. The effect of such a decision will be that (a) more Medicare patients will die from colon cancer, and (b) the costs of Medicare will continue to escalate because Medicare will be paying for treatment and care of colon cancer patients, rather than preventative care for an extremely curable disease.”
For more information: https://www.cms.hhs.gov/mcd/viewpubliccomments.asp and http://www.powelltate.com/websites/mita/miu/vc_video.html

 February 06, 2024
February 06, 2024 









