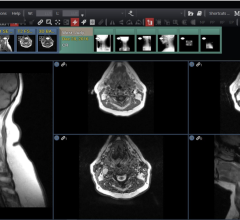
Closed loop imaging will optimize the set up electronically treating the scanners and injectors as IT devices driven by the protocoling tool.
When does the imaging clock start ticking? Is it when an image is taken in the scanning suite or when it reaches the PACS in the reading room?
According to a new study on imaging workflow, the imaging loop begins when the physician orders an imaging exam and only ends when the results of the test are communicated to the doctor.
Because optimizing radiology workflow requires seeing the big picture, a first-of-its-kind closed loop imaging research trial is taking a holistic approach toward restructuring the imaging process.
Conceptualized and lead by Paul J. Chang, M.D., FSIIM, vice chairman of radiology informatics and medical director of pathology informatics at University of Chicago Medical Center (UCMC) and working in collaboration with Philips Healthcare, the study’s objective is to reduce errors and improve quality of care and patient outcomes.
UCMC and Philips are working together to integrate the technologies to automate tasks, improve workflow efficiency and ultimately optimize care.
During the initial research phase, UCMC replaced the current paper-based CT protocol system manual entry of a list of images requested, as well as contrast and dose requirements, with an automated electronic patient protocol system that uses a Philips tablet PC for wireless access to relevant patient and scanning protocol information. Protocol settings are automatically communicated to the CT scanner, simplifying CT scanning by sending all relevant clinical information and protocol definition without requiring manual entry. Event-driven alerts provide updates throughout the entire imaging process and notify radiology staff when images are ready for processing. Overall, the radiology department was able to eliminate non-essential work and paper trails.
Total information throughput
Imaging Technology News had the opportunity to speak with Dr. Chang about his perspective of radiology workflow and strategies for streamlining the bottlenecks.
ITN: PACS companies have been trying to improve upon radiology workflow for several years. What are the factors driving your quest to improve processes in radiology?
Dr. Chang: I noticed that PACS companies in general, along with speech recognition companies and the integration of speech recognition, basically have resulted in incredibly efficient and very optimized reading rooms. But, here’s the problem, it doesn’t matter how efficient we are in the reading room if the rest of what we do in radiology is inefficient. I can be incredibly accurate in radiology in the reading room, but if the study was not acquired accurately, it’s the old ‘garbage in, garbage out.’
The concept started with this closed loop imaging a number of years ago when I started talking about this concept of total information throughput as a measure of how we’re doing in the radiology department. When we as radiology administrators judge how we’re doing, we’ll talk about patient throughput in our department, report turnaround time. The problem is these are incomplete measures of how we’re doing in total, and that’s why I keep pushing this concept of the best way to measure how we’re doing in the radiology department is to look at total information throughput. The clock doesn’t start or stop in radiology, which a lot of these measures do.
What good is it to have a patient scanned in two seconds if I don’t read the study for four hours? We have to look at the entire loop and optimize at every stage of the game and like I said the clock doesn’t start and stop in the radiology department. It starts when the physician first decides that imaging might contribute to the patient care and only ends when that same physician gets my report or some other message from me with the result that hopefully can contribute to patient management.
The concept of the loop is that it begins not in radiology; the loop begins and ends with the patient. Closing that loop is the purpose of this project. The whole goal of this is to optimize the total information throughput, not just what goes on in radiology.
Optimization focus
ITN: What are some of the areas that need optimizing?
Dr. Chang: The whole purpose of closed loop imaging is to optimize the entire sequence. For the first time, we will look at all parts of this imaging cycle. Not just the ones in the radiology reading rooms, not just the ones in the imaging suite, but the whole process.
We have to improve the accuracy and quality of what we do.
Another axis is safety: reducing dose and improving what we do with respect to contrast.
Bottlenecks
ITN: The study is designed to remove inefficiency at all points within the imaging loop. What are some of the major bottlenecks and non-essential steps in the imaging loop?
Dr. Chang: The initial bottlenecks in the past were in the reading room because of PACS, RIS and integration of speech recognition. Yet the real bottleneck within radiology is in the scanning area.
A perfect example is protocol. Many of us use protocol sheets. To be optimal, you need two people to take that protocol sheet and do the right thing in the imaging suite — a radiologists who knows what needs to be done and who can communicate that to an engineer to set up the scanner.
But we have neither of those people. We have a technologist who we expect to play the role of a radiologist and an engineer at the same time and translate that into the protocol of the scanner and the injector. This takes a very long time because there are so many parameters in an MR scanner or an injector. Sometimes we will simplify the protocol – instead of 20 things we could do, we’ll reduce it to three to reduce the complexity and the set-up time.
The goal of the closed loop imaging trial is to have my cake and eat it too – I don’t care how complex a protocol is, it will get set up perfectly – both the injector and the scanner – and without negatively impacting efficiency.
The only way to do this is to treat for the first time the modality as an IT device. For the first time we have to view the scanning devices themselves as IT devices that have to be integrated.
So the system will automatically extract the lab values, the pathology reports, the history – not just get the requisition but get the clinical context from the EMR. Not requiring me to go to the EMR directly – it gives me a Web page that says here are the cases that need to be protocoled, here is the information right at my fingertips to allow me to use the right protocol.
Step two, identify the patient. The technologist is wasting time trying to identify the patient. So when the patient comes in with an RFID tag, the patient is automatically identified, the scanner automatically knows who it is, automatically checks the electronic protocol, and transmits that protocol in a language that the scanner and injector can understand natively – and set itself up. Now the technologist doesn’t have to do the busy work. So one of the aspects of this closed loop imaging is to optimize the set-up electronically – treating the scanners and injectors as IT devices driven by the protocoling tool. The closed imaging loop will include Medrad and their contrast injector system. They have all Web services.
ITN: What other steps will be automated?
Dr. Chang: Another step involves automating the post-acquisition workflow. The technologist is spending many minutes setting up the post-acquisition workflow – getting the thin slices set up, then manually pushing to 3D workstations. The more time that takes means we can’t scan the next patient, throughput is negatively impacted and it also increases the risk of error.
The next step is to build integrated coordination to allow the sufficient provisioning of resources, not just in the scanning suite but improve the overall coordination. We have to have a more efficient view of the overall operational coordination of who we scan or how we scan them. We need to give to the technologist or supervisor a tool or dashboard that lists all of our inpatients, and all of our outpatients, and then when we select that patient it automatically knows 15 minutes into the study to call for the next patient, call for transport, have the patient in the waiting room to start taking contrast.
Another part of this closed loop imaging initiative is to enhance the kinds of synchronous and asynchronous mechanisms we have to communicate to doctors. An asynchronous tool is a text messaging or tickler files that automatically notify the physician when there is an urgent result.
We want systems to make sure there is a safety net. That’s basically closed loop imaging. We have to take a total view of what goes on in radiology. We have to improve the bottlenecks, the bottlenecks in the scanning suite, the bottlenecks in communication, the bottlenecks in how to order.
Building on SOA
ITN: What healthcare language or standard will be used?
Dr. Chang: We have chosen for the first step to use the DICOM modality list because you have the provision to send the protocol. It is intensely under-leveraged. We have seen in our initial results, in order to drill down and improve the efficiency of the set-up automatically, we need to give the scanner more detail. So we are using service-oriented architecture (SOA) and Web services to do the same thing, and Philips has that architecture. That is one of the differentiating features Philips provides.
Here’s why I’m an advocate of SOA. In the world of SOA, view it as an organism. What we are building is a workflow engine that can take as services and orchestrate this complexity. If I got an RFID signal that a patient just came through the scanner, that information is sent to the scanner, the protocoler and the injector.
ITN: Is that why PACS will turn into a service?
Dr. Chang: Exactly. Everything is a service. So the first step is to expose everyone of these resources: PACS, 3D, modalities, RIS, EMR, CPOE, all of these things, as services. Web-services is the spinal chord and SOA is the brain. That’s what closed loop imaging is based on – SOA.
Closed loop imaging is an ongoing methodology that looks at the entire loop to improve efficiency, while optimizing quality and while optimizing safety – we have to have our cake and eat it too.


 July 25, 2024
July 25, 2024