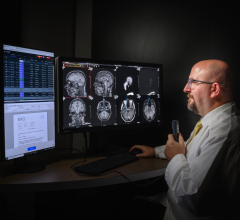
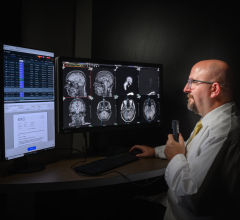
Dr. Robert Wells of Wisconsin-based Pediatric Diagnostic Imaging is shown at the Fusion RIS/PACS from Merge Healthcare
Some Web 2.0 tools are features commonly used among consumers to better communicate and gather information. Such tools are being adapted for and adopted by radiologists. Many radiologists already tap into instant messenger, digital reference libraries, access radiology chat rooms and more. But will these capabilities be added to the arsenal and integrated into the radiologist’s workflow and embedded into the next generation of RIS/PACS offerings?
To discern which Web 2.0 tools might enhance the radiologist’s experience, we examined the biggest challenges facing today’s RIS/PAC systems and what key capabilities could be added to a future RIS/PAC system.
At the Pediatric Diagnostic Imaging (PDI) center, founder Robert Wells, M.D., and a team of pediatric radiologists, nurses and technologists, work with a multimodality integrated RIS/PACS from Merge Healthcare to manage images generated by MRI, CT, ultrasound, fluoroscopy and general X-ray. Dr. Wells is a renowned and respected pediatric radiologist.
Dr. Wells spoke with Imaging Technology News regarding some of the biggest challenges with today’s RIS/PAC systems and what are important features to have in any RIS/PAC system. He also identified the features critical to the streamlining the radiologists’ workflow and identified capabilities that are lacking in today’s standard RIS/PAC system.
Cycling Time
An important consideration in a PACS workstation is the cycling time between imaging studies. When performing hundreds of interpretations a day, every few seconds of cycle time adds up to a lot of wasted time. Our current PACS has a fast cycle time.
RIS/PACS Integration
A second issue is having a fool-proof correlation between the images presented on the PACS viewing screen and the patient information on the radiology information system, to assure that the radiologist is dictating for the correct patient and study. That’s one of the advantages of having an integrated RIS and PACS — they should always correlate. Providing the interpreting radiologist with accurate clinical information always improves the quality and efficiency of the image interpretation process. The usefulness and quality of the radiologist’s report directly correlate with the quantity and quality of the clinical information that the radiologist has while viewing the study.
Presenting the Information
The better job a RIS/PAC system does at presenting information in a user-friendly manner, the more efficient the radiologist will be. There is a marked variation between vendors in regard to what information is gathered and how it is presented.
Finding Priors
Another factor is how efficiently a system presents information about prior examinations. It is important, first of all, to know if there was a prior examination. Then, I want to be able to view the report quickly. The system should make it easy to compare the images of the new and old exams. Our system does a good job of presenting prior studies, but many PACS fall short. I work with another PACS that doesn’t give you any clue that there was a prior study. You have to guess that there might have been one or rely on a heads up from the technologist, and then use the patient i.d. number to manually search the PACS records. In addition, you have to close the exam that you are looking at in order to perform the search. That is one example of a system that is extremely “user unfriendly”.
The system we use from Merge presents on the main screen a list of everything we have ever done on that patient; the information is at your fingertips, and the images are immediately available.
3D Capabilities
Some radiology practices may rely on 3D capabilities more heavily than we do. The nature of our work does not require it. Having 3D capabilities is a useful feature, but I don’t consider that to be a crucial workstation feature. When we do need 3D image presentation, we have the technologist set up the study on another workstation. I would rather not have to go through the process of manipulating the images.
Worklist Protocols
It can be useful to have the ability to manage the worklist protocols to correspond to your personal workflow. Customizing your worklist is particularly important in a large practice. Also, being able to readily identify cases that need to be looked at immediately is important. If there are multiple radiologists working concurrently, being able to automatically direct to the appropriate radiologist is useful.
Critical Results
An optimal PAC system would have an embedded solution for critical results reporting and documentation. It would present you readily with the appropriate person and phone number to call, and then have a simple way of documenting that you made the call, and then be able to provide a confirmation of the call. Some PACS vendors are considering embedding this functionality. Currently, we document critical results on paper. I believe there is at least one vendor offering software to manage critical results documentation.
Quality Assurance
Another potential ancillary RIS/PACS function, like a critical results management solution, is quality assurance. It would be nice to have it embedded in the system. One of our main QA techniques is to review the images and report from prior studies during the routine interpretation of current exams. Instead of filling out a data entry card or jumping to another computer screen, it would be useful for the RIS/PACS to present with a text box to click on in order to indicate agreement or disagreement with what the interpretation of the prior radiologist. This technique meets quality assurance criteria. It would be more efficient to have the radiologist response opportunity embedded. Another ancillary function, is the ability to mark a case for future reference and record comments about why you are saving it, and then being able to easily retrieve those cases for teaching or QA.
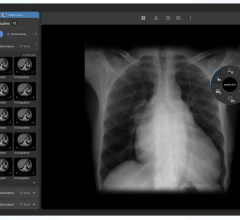
Image Interpretation Tools
For the PAC system itself, the image interpretation process should be a simple, rapid technique. Efficient use of the various tools is important — being able to pull up the zoom or pan features, or change the layout or magnification, or change the window and level. You don’t want to have move through multiple venues to get the tool you need. This is made more difficult by the presence of so many tools in a modern PACS — you have to pick one off a list of 40 choices. All the vendors are coming up with ways to address this problem, but the solutions that I have seen are all a little bit cumbersome.
Those of us who use multiple PAC systems suffer with the problem of inconsistency of functions. The right mouse usually does one thing on one system and it does something different on the other. That can be very difficult, since it is distracting to have to stop and think about which button to push. The mouse controls from different PACS usually do different things – this slows down the image evaluation process for the radiologist. For instance, on the system that I usually use, the right mouse controls window and level; but on another system that we use, the middle button controls window and level, and if I accidentally click the right mouse, it takes me to a menu that is very hard to get out of again. Not all systems are easily customizable to instruct the mouse on what specific commands to use. The more user-customizable the controls are, the better the system.
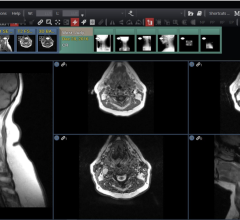
Hanging Protocols
Functional hanging protocols is another issue. The concept of hanging protocols sounds good, but in day-to-day practice they are often so difficult to set up or they fail so frequently, that many disable the function.
Interoperability
Interoperability can be an issue particularly from different modalities. Some PAC systems have trouble with the images coming from different modalities, or from modalities from different vendors. On our Merge system at our imaging centers we have no troubles, but I have observed problems with other systems.
Viewing All the Images
Another feature of PACS that I think would be useful is feedback about whether you have viewed all the images in a study. You may be looking at a study that consists of one or two images, or 450 images. Your responsibility to the patient requires that you look at every single image. With the “old days” of X-ray films, it was easy to see the entire study hanging on the viewboxes, and readily identify everything you had to look at. Now, it is pretty easy to miss a series or some images in a series, unless the PACS gives you a simple way to cycle through all of them. With a good PACS, when you are closing the exam, it would be optimal to have a warning that you haven’t seen all of the images. I know this feature is on the radar screen of vendors. Although our system does not have this feature, it does have a simple system to cycle through the entire study.
Web 2.0 Tools
Our current RIS/PACS from Merge has the ability to send typed messages back and forth between radiologists – similar to instant messenger. Anyone signed in to a workstation can send and receive these instant messages. There are instances where it is more useful than the phone because the other person can finish what he/she is doing before responding. Also, you can give them typed information, such as a name or number that is more cumbersome to give over the telephone. The message sits on the receiving radiologist’s screen until he/she responds. We find this is a useful way to communicate even when there are only two people working, but would be especially helpful with several radiologists working at different sites.
Decision Support Tools
Decision support tools are either a reference to a peer review journal or reference to images of similar cases. For many radiologists and residents, the modern technique to search for reference information is to access Google. People don’t get up and refer to a book anymore. It would be quite useful to have something more than what Google provides, which is looking for the diamond in the rough. In many instances, Google may find pertinent abstracts, but you aren’t allowed to see the full text and images. While there are free radiology reference sites such as MyPACS.net, where findings by radiologists are uploaded, and Yottalook.com, the Google site for radiology, Dr. Wells added that there is something lost by radiologists not using books.
Lots of times the information on the Internet is superficial or just flat out wrong. The physicians in training rely so much on the Internet and have given up on using reference books. I think that the combination of the two is probably optimal – using the web to supplement reference books. The Internet by itself is not a complete substitute for textbooks and journals.
Reference: Robert G. Wells, M.D., founder of Pediatric Diagnostic Imaging, holds an associate clinical professor position at the Medical College of Wisconsin and has been active in the pediatric radiology community for over 20 years. He is active in medical student, resident and fellow education. Dr. Wells has published numerous scientific articles and book chapters. He also coauthored a comprehensive pediatric radiology textbook. He is a frequent participant at conferences, seminars and other educational meetings.


 July 25, 2024
July 25, 2024