Edward Cancer Center, Naperville, IL
Clinicians at Edward Cancer Center in Naperville, IL are using a Trilogy system from Varian Medical Systems to offer cancer patients image-guided stereotactic body radiotherapy (SBRT), and also to adapt treatments as the tumor responds, sparing more healthy tissues and, in some cases, making radiotherapy a viable option where it would not have been.
Vasudha Lingareddy, M.D., medical director of the Edward Cancer Center Department of Radiation Oncology, described a recent case of small cell lung cancer that involved delivering just enough dose to shrink the tumor, watching for the tumor response, replanning at a critical point for maximum sparing of normal tissues and replanning again to spare the spinal cord as it approached its dose tolerance.
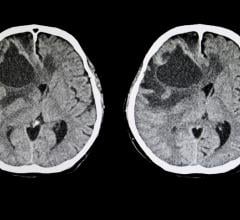
The 69-year-old former smoker had developed a persistent cough and wheezing. A CT scan in November 2006 revealed a large right hilar mass. “It was seven centimeters — that’s large,” said Dr. Lingareddy. “The next question was, what type is it, small cell or nonsmall cell?” Several fine needle biopsies came back atypical, but were inconclusive. A surgical biopsy finally revealed that she had small cell cancer, which tends to grow quickly and metastasize; however, it often responds well to radiotherapy.
Many patients with small cell lung cancer are first given two cycles of chemotherapy prior to radiotherapy. But in this case, a repeat CT scan revealed that the mass was growing quickly and already occluded the right mainstem bronchus. “Her respiration was becoming seriously compromised, so we decided to go ahead immediately with radiation, to reduce the tumor volume as quickly as possible,” Dr. Lingareddy said.
Prior to planning the treatment, Dr. Lingareddy ordered a PET/CT study. “This was crucial because it was difficult to tell where the tumor ended and the collapsed lung began,” she said. “We were able to visualize the active parts of the tumor, and more importantly, we found a satellite nodule along the pleura,” a thin covering that surrounds the lungs.
Dr. Lingareddy worked with John Fan, Ph.D., senior medical physicist, to create the treatment plan. “I contoured her normal lungs (right, left and total), heart, tumor volume, spinal cord. We started out with anterior/posterior fields to spare as much lung tissue as possible, but we knew that the volume of lung inside the treatment fields would be a problem. With our first plan, nearly 40 percent of the lung was receiving 20 Gy or more, and you generally want to keep that under 25 percent. But we tried other field arrangements and couldn’t do better. The patient consented to a treatment that might make her
oxygen-dependent. However, knowing that we were dealing with small cell lung cancer, we were hoping for a good response that would make it possible for us to replan her before her lung tissues reached tolerance levels.”
Imaging to Position the Patient for Treatment
Dr. Lingareddy’s clinical team used the Trilogy system’s On-Board Imager each day to position the patient for treatment. “We had elected not to place fiducial markers, so we used kV/MV image matching to line up soft tissue and bony structures. The mass was clearly apparent so it was easy to make the matches.”
The Trilogy system’s PortalVision MV imager was also used in cine mode to generate movie loops of the treatment fields during the first two treatments. “Those images showed the respiratory motion and allowed me to assess whether I had adequate margins,” Dr. Lingareddy said. Since then, Edward Hospital has added CT with gating — 4D CT — so that treatment plans can account for tumor motion from the outset.
Dr. Lingareddy’s clinical team began delivering 1.8 Gy per fraction, a low dose chosen because of the patient’s concurrent chemotherapy — she was receiving taxol and carboplatin — as well as the size of the tumor volume.
Cone-Beam CT Reveals When to Replan
On January 16, 2007 — two weeks into the treatment — Dr. Lingareddy checked to see if the treatment fields could be reduced. “We used the On-Board Imager to generate a cone-beam CT when her lungs were reaching 16 Gy because beyond 20 Gy, it would have been too late,” she said. “At 16.2 Gy, the GTV (gross tumor volume) had shrunk significantly. We were able to shrink the field size from 13.2 by 14.6 centimeters down to 11 by 9 centimeters. That reduced the volume over 75 percent, from 450 cubic centimeters to 104.6 cubic centimeters. The patient was elated.”
But Dr. Lingareddy wasn’t finished with her adaptations. “At some point, we needed to come off the spinal cord,” she said. “With concurrent chemotherapy, we have to be even more conservative than usual, so I wanted to keep spinal dose under 45 Gy. When we were approaching that dose level, we switched to a set of oblique fields that avoided the spinal cord altogether. We created a three-field plan: left anterior oblique (LAO), right posterior oblique (RPO), plus a left lateral field to bring the dose in more laterally. This actually improved the dose coverage.” Whereas the first plan had nearly 40 percent of the lung receiving 20 Gy or more, when the three plans were summed, only 21 percent of the patient’s lung finally received that much dose. “Making those adaptations enabled us to save more of her normal lung tissues,” Dr. Lingareddy said. “It meant the difference between being oxygen dependent or not.”
According to Dr. Lingareddy, the steps involved in adapting a radiotherapy plan based on images were greatly facilitated by the tight integration of the elements that make up the Trilogy treatment system she uses at Edward Cancer Center. “There are other technologies that would allow you to do daily imaging, but this system makes it easy to use those images efficiently. Simulation is tightly integrated with treatment planning, imaging and treatment delivery. Once we acquire the 3-D image, we can quickly and easily visualize the tumor response and use that information to modify the treatment plan. It’s very efficient for the patient as well as for us and very accurate.”




 September 12, 2025
September 12, 2025