Source: Agfa Healthcare
With all the discussion surrounding the development of a national Electronic Health Record (EHR), perhaps nothing better demonstrates this need than the events that unfolded on the Gulf Coast last September. When Katrina raged ashore and left a wake of destruction, government and industries struggled to regain footing. The stories of stranded and vulnerable citizens and hospital patients struck a social cord across the U.S. However, an opportunity was created, one that received a timely response.
Last November, the U.S. Department of Health and Human Services (HHS) announced it entered into agreements to support digital health recovery for the Gulf Coast. “Recent hurricanes in the Gulf Coast exposed up-close the real vulnerabilities of the American healthcare system — a system based upon paper which in an instant was destroyed,” said HHS Secretary Mike Leavitt. “The effect of these hurricanes has been to demonstrate the real need for health records that are both electronic
and interoperable.”
The agreement created a task force of local and national experts to help implement, support and disseminate state-of-the-art information technology that will contribute to an infrastructure that supports interoperable healthcare data exchange. The State of Louisiana Department of Health and Hospitals will develop a prototype of health information sharing and EHR support that can be replicated throughout the region.
Integrating Disparate IT Systems
The prevailing thought surrounding a nationwide or geographical cluster of the EHR is not as one large repository of health data, according to H. Stephen Lieber, CAE, president and CEO, Healthcare Information and Management Systems Society (HIMSS), but that the information will reside at a hospital or physician level and be made available to authorized users upon request. This will minimize security issues and ensure that information is accessed on demand.
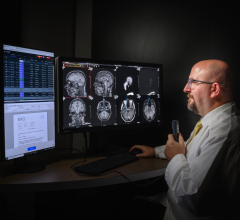
Such a concept will rely upon disparate clinical and administrative systems working in tandem to bring together all pertinent aspects of a patient’s prior and current health information in a timely manner. It also implies that existing department- or specialty-based IT solutions must migrate to a broader IT infrastructure. In the radiology department, this could evolve into the launch of the image-enabled EHR.
“This is a new day, and we must understand [the need] to integrate images into the EHR,” said C. Peter Waegemann, CEO, Medical Records Institute. As the leader of the organization that spearheads the annual Toward an Electronic Patient Record (TEPR) conference, Waegemann understands all too well the need for the EHR/EPR (electronic patient record) industry to integrate with department-specific solutions like PACS and RIS.
Getting there is half the battle according to Waegemann and David Merritt, project director, Center for Health Transformation (CHT). While Merritt concedes much progress has been made with radiology IT systems, he noted that “one of the key problems [remains] the lack of data standards to allow different systems to share information.” Waegemann agreed that current standards such as DICOM, HL-7 and the IHE are good starts, saying, “They are moving in that direction very slowly.”
Another issue that Merritt believes is more important than standards is getting technology into the hands of the providers. “The best result I’ve seen from any study is that 20 percent of physicians actually have some type of health information technology. [However], even if a hospital system has a very robust, advanced system, it won’t matter if the institution is in a silo with no one connected. Without the technology, the whole standards debate is just moot.”
Education is key to helping clinicians understand the value of health information technology, Waegemann stressed. “The industry must understand the potential of integrated health systems,” he said. For more than 21 years, this has been the goal of Waegemann and the Medical Records Institute’s TEPR conference and exhibition. For 2006, TEPR is changing its educational programming to reinforce this message to clinicians, nurses and other healthcare providers in facilities of all sizes.
Yet, Merritt noted that political and economic barriers hinder the adoption of health information technology, a necessary first step on the road to an integrated EHR. Many small group practices or solo practitioners simply cannot afford health information technology. Third-party payers have not stepped up to the challenge to help their in-network physicians. Further, he pointed out that the government has yet to initiate any discussion for providing incentives to clinicians who invest in health information technology, even though the federal government continues to emphasize the need for a nationwide EHR. Finally, Merritt noted that breaking down obstacles such as laws prohibiting hospitals from providing IT systems to local physicians is “a very important policy priority” for the center.
“The technology is out there, that is the easy part,” Merritt added. “It is the intangibles, changing physician behavior or health plan strategy that will be difficult to resolve.”
Image-Enabled EHRs
The explosion of diagnostic imaging and its important role in determining clinical pathways is vitally important to the future of the EHR. “We can have the best imaging system in the world that can detect conditions at a very early stage,” Merritt explained. “If that information is static and not shared, we miss the point of technology.”
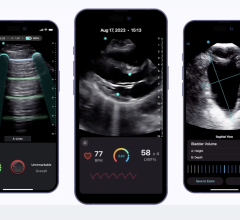
Waegemann agrees, but takes the vision a step further. “The [electronic] image part of the clinical record is not just for specialists, it is independent of the medical device or computer being used. In the future, any authorized pediatrician or family physician must have access to the image, even if on a small display or handheld device.” He believes that the EHR must be integrated with diagnostic images, and that success in this arena is dependent upon the integration of medical and clinical documentation.
Both Waegemann and Merritt agree that the image-enabled EHR will further propagate use of teleradiology. With the advent of the Internet and recent industry investment in fiber optic cable, past barriers such as high-speed data transmission of images are minimal. In fact, Waegemann, sees the broader picture of telemedicine as “[j]ust one of the ways to communicate between two medical parties, imaging or other specialties, to interpret information.”
CHT also foresees greater advantages in conjunction with telemedicine. “We envision modernized systems that are completely connected, so that every stakeholder can share the information that they need to properly care for their patient,” Merritt explained. The goal is to utilize health information technology at the point of care to improve decision making on treatment options. He cautions, however, that information technology is not an end in and of itself.
“We look at the research capabilities of an advanced system as being the real payoff. When we have the ability to capture patient data electronically, including images, we can then aggregate that data and see things that can’t be found thumbing through paper-based files,” Merritt said.




 June 28, 2024
June 28, 2024