May 25, 2016 — Researchers at Haukeland University Hospital in Bergen, Norway, have combined a laboratory ultrasound technique with the commercially-available chemotherapy compound Gemcitabine to increase the porosity of pancreatic cells with microbubbles. The technique is designed to help get the drug into cancer cells where it is needed.
Initial results were presented at the Acoustical Society of America’s 171st meeting, May 23-27 in Salt Lake City, based on the outcomes of a phase I clinical trial involving 10 people undergoing treatment for pancreatic cancer. They found the new approach nearly doubled the median survival time from 7 months to 18 months without increased chemotherapy dosage and with no added toxicity or additional side effects.
“When we compared the amount of treatment our patients were able to undergo, compared to a historical cohort, we saw a significant increase of treatment cycles,” said Spiros Kotopoulis, a researcher at National Centre for Ultrasound in Gastroenterology at Haukeland University Hospital in Bergen and The Departments of Clinical Science & Medicine at the University of Bergen, where some of his collaborators are also based.
Before the technique is proven effective, approved for routine care and made widely available to patients with this type of cancer, it must undergo further testing in clinical trials involving more patients — something that may take years. Nevertheless, these results are promising for a disease with an often poor prognosis. The one-year survival rate for all stages of pancreatic cancer combined is 20 percent, and the five-year survival rate is 6 percent, according to the American Cancer Society.
The concept of delivering payloads via ultrasound, sonoporation, has been around for decades, and was initially used to enhance gene uptake. Kotopoulis became involved while working on his doctorate at the University of Hull in the United Kingdom, ultimately delving into interactions between cells and bubbles during short bursts of ultrasound exposure.
During that time, a collaboration with a group of French biologists led to the technical development of forcing single microbubbles into a cell with ultrasound — opening the door to forcing any number of other compounds into the cell. As one of the largest barriers to a drug’s efficacy is its ability to permeate a cell membrane, this was a significant development — one Kotopoulis took with him to a postdoctoral fellowship in Bergen, translating the laboratory concepts to a clinical bedside.
For their phase I clinical trial, Kotopoulis and his colleagues recruited a cohort of 10 volunteers who had locally advanced or metastatic pancreatic adenocarcinoma. To facilitate more rapid clinical translation, the researchers and clinicians agreed to use technology and materials already available on the market at every step.
“If this worked, in 20 years, we didn’t want a hospital to have to purchase specialized, expensive, one-use equipment,” he said.
Their equipment consisted of a slightly older clinical diagnostic ultrasound scanner, the GE Logiq 9, combined with a 4C abdominal ultrasound probe. Using a diagnostic ultrasound scanner also allowed them to see and treat the tumor in real time. To generate the microbubbles, the researchers used SonoVue, a sulphur hexafluoride-based solution commonly used to help diagnose liver lesions through ultrasound. Since the bubbles are only stable in the blood stream for a few minutes, the researchers decided to inject a small amount every three and a half minutes.
For chemotherapy, the researchers used a drug called Gemcitabine.
“At the time, this was the best option for extending survival in patients with pancreatic cancer,” Kotopoulis said.
The clinicians began the procedure by administering standard chemotherapy to the patients according to the existing protocol. Once the chemotherapeutic concentration in the blood reached its maximum, the researchers used the ultrasound scanner to induce sonoporation for 31.5 minutes, at 3.5-minute intervals.
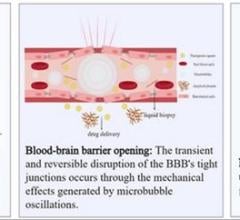
According to Kotopoulis, the microbubble’s permeability-enhancing mechanism of action is somewhat opaque, but is believed to be one of two methods.
At high acoustic pressures, microbubbles undergo inertial cavitation — an implosion that creates tiny pores in the cell, allowing a greater concentration of drugs to enter. This effect, which includes shockwaves, may penetrate deeper into the tissue, thus having a deeper effect. Due to potentially violent ripple effects — similar to throwing a cannonball against a wall — this is generally avoided, Kotopoulis said.
At low to moderate acoustic pressures, the bubbles tend to interact with cells, bouncing and rolling against them to push and pull the membrane, occasionally entering the cells — more akin to cracking open a safe by drilling some small, precise holes.
When treated with sonoporation, the volunteers were able to undergo 14 (±6) cycles of treatment, versus 8 (±6) with normal chemotherapy.
This ultimately had the effect of stabilizing or decreasing the tumor volumes in 50 percent of the patients and increasing the median patient survival time from approximately 7 months to 18 months.
Future work for Kotopoulis and his colleagues will include performing a larger-scale phase I/II clinical trial with international collaborators, and working to develop a microbubble compound optimized for targeted drug-delivery at low acoustic intensities. They will also seek to fully understand the mechanisms of sonoporation by using advanced mouse models and bioreactors.
For more information: www.acousticalsociety.org


 July 19, 2024
July 19, 2024