August 29, 2012 — The ability of magnetic resonance imaging (MRI) to create exquisite images of the body’s soft tissues – and the tumors that arise amid them – is helping physicians at National Cancer Center Singapore (NCCS) to precisely shape brachytherapy doses to cervical tumors, while at the same time avoiding exposure to critical healthy organs and tissues.
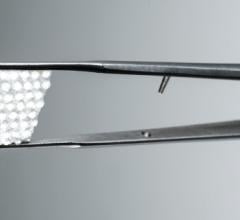
Since November 2011, NCCS clinicians have used MRI to characterize soft tissues, organs at risk and lesions before successive brachytherapy treatments using the microSelectron Digital remote afterloader and Oncentra 3-D Brachy Image-Guided Treatment Planning system, both manufactured by Nucletron, an Elekta company.
Brachytherapy is an advanced, highly targeted cancer treatment in which radiotherapeutic sources are placed in or near a tumor, giving a high radiation dose to the tumor while reducing the radiation exposure in the surrounding healthy tissues. NCCS uses microSelectron Digital high-dose rate (HDR) brachytherapy, which introduces the radiation source for a certain time using a special applicator.
“After our first year using CT [computed tomography]-based planning for 3-D brachytherapy, we felt confident enough to take the next step: MRI-guided adaptive brachytherapy,” said Richard Yeo, M.D., senior consultant radiation oncologist at NCCS. “The ability to visualize the tumor on MRI and plan the treatment ‘live’ is nothing short of amazing.”
Better images, better treatment
MRI provides information about the tumor’s volume (3-D) and how the volume and shape change between treatment sessions (4-D). Performing an MRI scan before each brachy session enables clinicians to adapt the dose to the unique anatomy of each patient, accounting for not only the position of organs at risk, but also tumor regression or movement, which may have occurred during preceding external beam radiotherapy and/or chemotherapy, and between brachy sessions themselves.
Conforming brachytherapy doses closely to the tumor’s shape and position is important in order to apply the highest possible dose to the tumor while limiting the dose to critical structures such as the bladder and rectum, thereby decreasing the likelihood of treatment side effects.
“The Oncentra Treatment Planning [OTP] system is very user friendly, with its intuitive interface and flexible workflow for managing CT and MR images,” said Lawrence Ng, consultant physicist at NCCS. “The recently upgraded OTP version 4.1 incorporates a very useful 3-D modeling library for accurate applicator placement during planning. This results in enhanced accuracy in source dwell position reconstruction and dose calculation, which hopefully will translate into better treatment result.”
Various publications from leading hospitals around the world have shown that use of this advanced technology allows healthcare teams to treat even the most complex cervical cancers, expected to result in lower recurrence rates and higher survival. Intensive multicenter research is ongoing, with the aim to provide more data to confirm these treatment benefits over traditional methods. This will allow experts to address unmet medical needs for this common cancer.[1]
World-class training
A group of NCCS experts received training on MRI-guided adaptive therapy at the University Hospital of Vienna, a leading center pioneering the development of this technique for the treatment of cervical cancer. The advanced work done in medical centers in Austria, and across Europe, will now gradually be adopted in a growing number of hospitals in the Asia Pacific region.
“Building a network of regional expertise will help other Asian hospitals adopt this new technology and provide state-of-the-art treatments to their patients,” said Ulrich Krumme, regional director, sales and marketing, Elekta Brachytherapy Far East. “This will be especially important, as technologies that have been developed in Europe will need to be adapted to local infrastructures and patient demographics. The potential clinical benefit of 3-D gynecological planning and treatment over the conventional 2-D approach makes it attractive for us to help hospitals with the adoption.”
For more information: www.nucletron.com/oncentra
Reference:
1. Radiotherapy and Oncology 94 (2010) 173–180, Int. J. Radiation Oncology Biol. Phys., Vol. 65, No. 2, pp. 624–630, 2006, Clinical Oncology 22 (2010) 602-604.


 July 11, 2024
July 11, 2024