June 18, 2014 — Anti-androgen hormonal therapy, also called chemical castration, can be an important defense against further disease progression for patients with prostate cancer that has traveled and grown in other areas, or metastasized, but some cases simply do not respond to this treatment. A new molecular imaging agent has been developed to help clinicians find as much cancer as possible, whether it is responding favorably or not, in an effort to improve clinical decision making for these patients, said researchers at the 2014 annual meeting of the Society of Nuclear Medicine and Molecular Imaging (SNMMI).
The imaging technique in the study is called F-18 DCFBC PET/CT, developed at Johns Hopkins University in Baltimore, by study co-author Martin G. Pomper, M.D., Ph.D. F-18 DCFBC is a unique small-molecule PET (positron emission tomography) agent that searches for and attaches to prostate-specific membrane antigen (PSMA), which signals more strongly from malignant prostate cells than from normal cells. The study further proves the effectiveness of the imaging agent by providing substantial clinical data for both castration-sensitive and castration-resistant prostate cancer patients.
“Currently there is a great unmet need in prostate cancer management and drug development for a functional imaging agent that is able to detect prostate cancer and monitor response to therapy,” said Steve Cho, M.D., Ph.D., assistant professor of nuclear medicine and PET in the department of radiology at Johns Hopkins University School of Medicine. “Unfortunately, a truly reliable functional imaging agent for prostate cancer does not exist, but several exciting metastatic cancer imaging agents have been in development over the last several years. We are working toward improvements beyond the current capabilities of conventional bone and CT [computed tomography] imaging, and a small-molecule PSMA-based PET radiopharmaceutical such as F-18 DCFBC is one such possibility.”
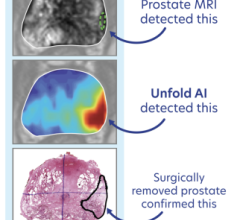
The agent is injected prior to PET imaging, and the particles emitted by the radiolabel, fluorine-18, are then detected by a PET/CT scanner. This hybrid imaging system uses both functional and structural data to create a composite image of anatomy and physiology with “hot spots” where the imaging agent is binding to PSMA targets in the body, otherwise known as tumor uptake.
This study includes the first 12 patients from an ongoing trial, including five cases of castration-sensitive and seven cases of castration-resistant cancer, both with rising PSMA levels and evidence of metastases. Hot spots representing tumor uptake were correlated with serum prostate-specific antigen and folate levels as well as castration-resistant status.
Results of the study showed F-18 DCFBC uptake was comparable to conventional imaging in relation to the lymph nodes, some bone and viscera, including the adrenal glands and pancreas. Lower DCFBC uptake was seen in highly scarred bone metastases when compared to other kinds of growths, but DCFBC PET was found to be more sensitive than conventional imaging for detecting bone metastases, especially within the cervical spine and areas showing degenerative changes, as well as in subcentimeter-sized lymph nodes. Additionally, a higher uptake of the agent was observed in castration-resistant bone metastases, and a direct link was found between PSMA levels and tumor-agent uptake. Further studies are required to get a comprehensive picture of the value of F-18 DCFBC PET for this patient population.
For more information: www.snmmi.org


 July 30, 2024
July 30, 2024