January 25, 2012 — Preoperative magnetic resonance imaging (MRI) helps surgeons make more informed decisions about nerve-sparing procedures in men with prostate cancer, according to a new study published online in the journal Radiology.
Excluding skin cancer, prostate cancer is the most common cancer diagnosed in American men, according to the Centers for Disease Control and Prevention. Open radical prostatectomy, or removal of the prostate, is a common treatment for the disease, but it carries substantial risks, including incontinence and impotence.
“I think preoperative MRI will be useful for surgeons who are uncertain whether to spare or resect the nerves,” said Daniel J. A. Margolis, M.D., assistant professor of radiology at the David Geffen School of Medicine at the University of California Los Angeles. “Our surgeons feel that, compared with clinical information alone, MRI is worthwhile for all patients, because it identifies important information leading to a change in the surgical plan in almost a third of patients.”
Robotic-assisted laparoscopic prostatectomy (RALP) is a newer treatment performed with the assistance of a surgical robot. RALP uses smaller incisions than those of open radical prostatectomy and offers improved cosmetic results, less blood loss and briefer postoperative convalescence. However, surgeons performing RALP lack tactile feedback, which may compromise their ability to evaluate neurovascular bundles; the collections of blood vessels and nerves that course alongside prostate. An aggressive surgical approach could unnecessarily damage the bundles and leave patients with loss of function, while an approach that is not aggressive enough may leave some cancer behind. There are no conventional preoperative urological techniques that provide information to take the place of tactile feedback.
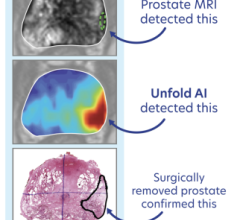
Dr. Margolis and colleagues investigated endorectal coil MR imaging as a way to improve preoperative assessment of prostate cancer and the involvement of the neurovascular bundles. They prospectively evaluated 104 prostate cancer patients who underwent preoperative endorectal coil MRI of the prostate and subsequent RALP. The researchers determined the differences in the surgical plan before and after review of the MRI report and compared them with the actual surgical and pathologic results.
Preoperative prostate MRI data changed the decision to use a nerve-sparing technique during RALP in 28 (27 percent) of the 104 patients. The surgical plan was changed to the nerve-sparing technique in 17 (61 percent) of the 28 patients and to a non-nerve-sparing technique in 11 patients (39 percent). The decision to opt for nerve-sparing surgery did not compromise oncologic outcome.
Dr. Margolis cautioned that the study group represented a population of men with low to medium grade cancer and that the findings might not apply to all patients.
“There is a learning curve for prostate MRI,” Dr. Margolis said. “What we and others have found is that one has to select patients where there is likely to be a benefit from the imaging.”
For the approach to become more commonplace, Dr. Margolis said that two things were needed: a better way to stratify which patients would benefit from preoperative MRI, and a more standardized means of acquiring and interpreting prostate MRI results.
For more information: www.radiologyinfo.org


 July 25, 2024
July 25, 2024