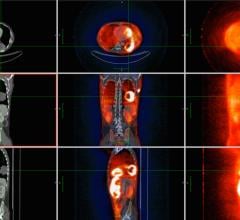
September 2, 2008 - Treatment plans using positron emission tomography (PET) were changed for more than half of patients, reported researchers in the largest multi-institutional study to date examining the impact of PET in changing disease management of individuals with suspected recurrent colorectal cancer, which appears in the September issue of The Journal of Nuclear Medicine.
The study was conducted at four sites throughout Australia and comprised 191 patients who were divided into two groups. Group A consisted of symptomatic patients who had residual structural lesions suspicious for recurrent tumor after initial therapy. Group B comprised patients with pulmonary or hepatic metastases that were potentially operable. These results were compared with findings from conventional imaging (such as computed tomography or CT), and participants were followed for 12 months.
"Designed with an evidence-based approach, this study confirmed the important role PET plays in the decision-making process of patients with colorectal cancer and the impact of PET on both the management and outcome of disease," said Andrew M. Scott, M.D., director of the Centre for PET and the Ludwig Institute for Cancer Research, Austin Hospital, Melbourne, Australia. "These results are compelling and indicate that PET should be made more widely available to patients."
Based on the extent and progression of disease revealed by the scans, treating physicians changed the planned management in more than 65 percent of patients in group A and nearly 50 percent in group B. The researchers also found additional disease sites in 48 percent of group A and 44 percent in group B, providing valuable prognostic information about patients that allowed their stratification into curative or palliative groups.
"PET was able to identify those patients who had potential for long-term, progression-free survival and even a potential cure," said Dr. Scott. "Just as important, it identified those patients with aggressive disease, enabling them to avoid unnecessary treatment, such as surgery."
In the U.S., imaging results from PET scans have also changed clinicians' decisions in the treatment and care of more than one in three cancer patients, according to data collected by the U.S. National Oncologic PET Registry (NOPR).
The registry "which was formed at the request of the Centers for Medicare and Medicaid Services (CMS)" has found that PET prompted changes in care decisions in 36.5 percent of patient cases. The study has to date included over 23,000 patients in more than 1,200 PET facilities nationwide. NOPR study data are collected through a clinical registry and provided to CMS to help determine levels of reimbursement for cancer indications not currently covered. CMS is currently reviewing the data to determine what additional types of cancer may be eligible for coverage.
"This data should encourage molecular imaging practitioners to engage with referring physicians early in the process of cancer treatment," added Dr. Scott. "It is clear that PET had a significant impact for these patients and could be an indispensable part of the standards of care for oncologists."
For more information: www.snm.org

 July 25, 2024
July 25, 2024