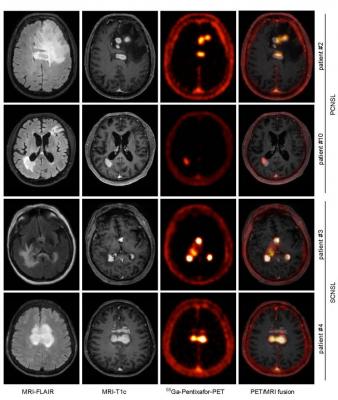
CXCR4-directed PET correlates with MRI-determined lymphoma lesions. Depicted are representative MR images (T1c- and FLAIR- sequences), and the corresponding CXCR4- directed PET images and fusion images (MRI-FLAIR and PET), of two patients with PCNSL and SCNSL, respectively. Images created by Department of Nuclear Medicine, School of Medicine, Technische Universität München, Munich, Germany.
December 14, 2020 — Positron emission tomography (PET) imaging with 68Ga-pentixafor is an effective diagnostic tool for central nervous system (CNS) B-cell lymphoma, according to a proof-of-concept study published in the December issue of The Journal of Nuclear Medicine. Targeting the CXCR4 biomarker involved in the growth, survival and dissemination of aggressive B-cell lymphoma, 68Ga-pentixafor PET imaging shows excellent contrast characteristics between lymphoma lesions and surrounding healthy brain tissue and may be suitable for risk stratification and response assessment.
"CNS B-cell lymphoma is a rare malignancy that has several clinical challenges, including diagnosis, risk stratification and optimization of treatment," said Ulrich Keller, M.D., Ph.D., head of the department of hematology, oncology, and tumor immunology at Universtitätsmedizin Berlin (Campus Benjamin Franklin), in Berlin, Germany. "Magnetic resonance imaging (MRI) is the current standard imaging technology for this disease, and while it provides high sensitivity, it offers only moderate specificity. Novel molecular and functional imaging strategies are urgently required for this patient population."
In a retrospective analysis to investigate this issue, 11 patients were imaged with 68Ga-pentixafor PET (four with PET/computed tomography and seven with PET/MRI). Lesions were analyzed, and immunohistochemistry was conducted. In the seven patients for whom post-treatment MRI scans were available, response to treatment was compared between the pre-treatment MRI and CXCR4-directed PET scans.
CXCR4-directed PET imaging with 68Ga-pentixafor was found to be positive in all active CNS lymphoma lesions, with a high tumor-to-background ratio that offered exceptional contrast. CXCR4 expression in vivo was validated by positive immunohistochemistry for CXCR4; in nine out of 11 patients for whom lymphoma biopsies were available, CXCR4 was highly expressed in the lymphoma lesions. Additionally, CXCR4-directed PET uptake values were found to have a significant prognostic value, indicating that lymphoma lesions with lower CXCR4 tracer uptake values were associated with a better response to standard treatment.
"This is significant for CNS B-cell lymphoma patients, as CXCR4-directed PET imaging with 68Ga-pentixafor could not only facilitate diagnostic work-up and response assessment but could also serve as a biomarker for selecting patients with a dismal prognosis who could benefit from more intense treatment options," noted Peter Herhaus, M.D., hemato-oncologist in the department for internal medicine III at the School of Medicine at Technische Universität München in Munich, Germany. "CXCR4-targeted theranostics thus moves nuclear medicine further on the track toward biomarker-informed molecular medicine."
For more information: www.snmmi.org


 July 31, 2024
July 31, 2024 








