Dec.11, 2024 — iCAD, Inc., a provider of clinically proven AI-powered cancer detection solutions, recently announced that four novel AI-driven breast cancer research abstracts were accepted for presentation at the 2024 San Antonio Breast Cancer Symposium (SABCS). These clinical abstracts highlight the latest research in breast health AI, focusing on improving detection and risk prediction accuracy and assessing disparities across diverse populations.
Presenting Author Chirag R. Parghi, MD, MBA, Chief Medical Officer at Solis Mammography, showcased three research abstracts — additional contributing authors include Jennifer Pantleo, R.N., BSN; Julie Shisler, BS; Jeff Hoffmeister, M.D., MSEE; Zi Zhang, M.D., M.P.H; Avi Sharma, M.D.; and, Wei Zhang, PhD.
Mikael Eriksson, PhD, epidemiologist at Karolinska Institute, Sweden, also presented research demonstrating a 10-year image-derived AI-risk model, based on iCAD’s ProFound Risk solution, for primary prevention of breast cancer showed higher discriminatory performance than the clinical Tyrer-Cuzick v8 risk model.
Advancing Breast Health with AI
“These studies exemplify the critical role the ProFound AI Breast Health Suite can play in not only improving early breast cancer detection and risk prediction but also in addressing health disparities in diverse populations,” said Dana Brown, President and CEO of iCAD. “We are proud to collaborate with Solis Mammography and Karolinska Institute contributing to groundbreaking research that can elevate the standard of care in breast health worldwide. These partnerships demonstrate the potential of our technology to improve patient outcomes, and also opens pathways to broader adoption of AI in healthcare, driving growth in key markets.”
Dr. Chirag Parghi, Chief Medical Officer at Solis Mammography, added: “These findings underscore the transformative potential of AI in empowering clinicians to improve outcomes regardless of age, race or breast density. By addressing traditional gaps in breast cancer detection and risk assessment, AI has the potential to exponentially improve current and future state breast cancer detection.”
Below are brief overviews of the poster presentations:
P2-06-20: Use of an AI Algorithm to Determine the Prevalence of Breast Arterial Calcifications in Women Undergoing Screening Mammograms Based on Race, Age, and Cancer Status (SESS-2141)
This poster explores the potential of an AI algorithm to identify Breast Arterial Calcifications (BAC), which are calcium deposits in the arteries of the breast that are commonly detected during routine mammograms. The study demonstrates that the weighted prevalence and distribution of BAC increases with age, as expected in a screening population. Interestingly, BAC prevalence did not vary by race, suggesting that it could serve as an effective cardiovascular biomarker across racial groups. Furthermore, the AI-based BAC detection algorithm highlighted a higher prevalence of BAC in women with mammographically detected breast cancer, suggesting women with increased BAC and breast cancer may benefit from cardiovascular assessment in addition to their oncological treatment. In that sense, a conventional mammogram could identify the cardiac needs of patients prior to or at the time of breast cancer diagnosis, providing an opportunity for early cardiovascular intervention.
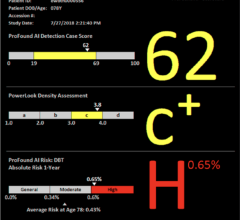
P2-06-24: Effect of an Image-Derived Short-Term Breast Cancer Risk Score in the Analysis of Breast Cancer Prevalence in Screening Populations by Race and Breast Density (SESS-2148)
This study delves into the development and validation of an AI-driven short-term breast cancer risk assessment score based on image-derived features, including mammographic density, and age. AI-generated case scores were shown to effectively stratify mammograms into categories with varying frequencies of cancer. The case scores did not vary significantly across racial subgroups in our dataset, suggesting that the accuracy of the AI software was consistent across races. The study concludes that an image-derived AI risk model is equally effective across race and density, providing accurate insight into short-term breast cancer risk. Based on the results, image-based risk scoring could offset known gaps in breast cancer detection by traditional mammography in patients with dense breast tissue and help address existing disparities across races. Findings from this study highlight the potential of AI to offer more consistent and equitable breast cancer risk assessments, improving both diagnostic accuracy and patient outcomes across diverse populations.
P2-06-25: Is Mammography Artificial Intelligence Consistent Across Race and Density? (SESS-2135)
This research focuses on the consistency of AI-based mammographic case scoring across different racial and breast density groups. The study emphasizes the potential of AI to provide equitable and reliable screening results, regardless of the patient's race or breast tissue density, two factors known to impact traditional mammography outcomes. For women with non-dense or fatty breast tissue, a low case score corresponded to a significantly lower frequency of cancer (1 in 11,363) compared to women with dense breast tissue who had a low case score (1 in 1,952). Although this finding was not statistically significant according to the Mann-Whitney U test, the difference between categories is notable, and the lack of statistical confirmation is likely due to the low absolute number of cancer cases in the low case score, non-dense cohort. Therefore, the negative predictive value of a low case score on a screening mammogram is presumably higher in women with non-dense breast tissue across a large dataset, suggesting a more reliable assessment for this group.
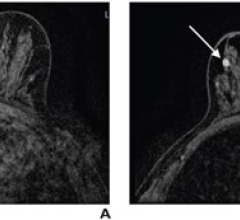
GS2-10: A Long-Term Image-Derived AI Risk Model for Primary Prevention of Breast Cancer
The research analyzed a two-site case-cohort of women aged 30-90 in a population-based screening study in Minnesota and the KARMA cohort from Sweden using an image-derived AI-risk model compared with the clinical Tyrer-Cuzick v8 model using clinical guidelines. Analyses were performed for risk of all breast cancer and restricted to invasive cancer alone. Using the National Institute for Health and Care Excellence (NICE) guidelines, considering women at 8% as high risk, 32% of breast cancers could be subject to preventive strategies in the 9.7% of women at high 10-year risk based on the AI risk model, the 10-year image-derived AI-risk model showed good discriminatory performance and calibration in the two case-cohorts and, showed a significantly higher discriminatory performance than the clinical Tyrer-Cuzick v8 risk model in KARMA. Demonstrating the image-derived AI-risk model has the potential for clinical use in primary prevention and targets up to one third of breast cancers.
For more information, including the latest in regulatory clearances, please visit www.icadmed.com.


 July 17, 2024
July 17, 2024