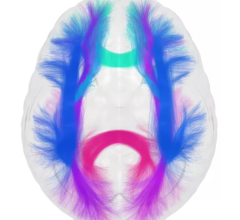
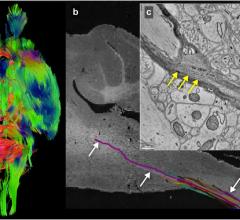
Cedars-Sinai neurosurgeons have begun using a high-definition imaging device to see inside the brain during surgery, allowing them to map safer pathways to reach and remove tumors. The device, called Brightmatter Guide, works like a GPS, providing real-time, brightly colored 3-D images that guide surgeons through the brain’s tiny neural connections while avoiding healthy tissue.
January 10, 2017 — Cedars-Sinai neurosurgeons have begun using a high-definition imaging device to see inside the brain during surgery, allowing them to map safer pathways to reach and remove tumors.
The device, called Brightmatter Guide, works like a global positioning system (GPS), providing real-time, brightly colored 3-D images that guide surgeons through the brain’s tiny neural connections while avoiding healthy tissue. Until now, neurosurgeons have relied largely on conventional magnetic resonance imaging (MRI) scans that provide flat, two-dimensional renderings of the brain.
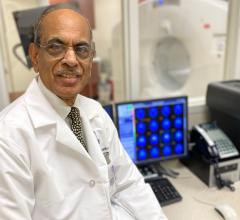
“This technology allows for us to more safely enter the brain without disturbing the important pathways connecting the brain’s critical areas of operation,” said Keith Black, M.D., chair of the Cedars-Sinai Department of Neurosurgery and director of the Maxine Dunitz Neurosurgical Institute. “An estimated 62,000 primary brain tumors and 150,000 metastatic brain tumors are diagnosed annually in the U.S. This new tool offers us a tremendous amount of hope for better outcomes for many of our patients.”
In a new video, available for streaming, Black demonstrates how the device works and explains how it may help neurosurgeons cut surgery time and improve patient outcomes.
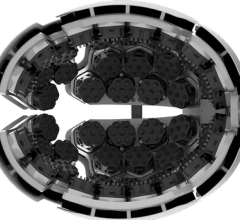
Cedars-Sinai is the first medical center in California to employ the new system. The device includes a camera that tracks the physician’s tools and shows a detailed image of the patient’s brain on a nearby screen. The tool can be used by surgeons operating on brain tumors, aneurysms, vascular lesions, skull-based issues and the spine.
Cedars-Sinai neurosurgeons perform approximately 600 brain surgeries a year. Going forward, about one-third of those procedures will be performed with the new device.
For more information: www.cedars-sinai.edu


 June 12, 2024
June 12, 2024