April 9, 2012 — New research published in the April issue of The Journal of Nuclear Medicine reveals that systemic inflammation causes an increase in depressive symptoms and metabolic changes in the parts of the brain responsible for mood and motivation. With this finding, researchers can begin to test potential treatments for depression for patients that experience symptoms that are related to inflammation in the body or within the brain.
Multiple studies in rodents have shown that inflammation in the body has effects on the brain. This has also been shown in a few human studies—both through measurements of behavioral changes and brain imaging—when subjects were engaged in various computer tasks. However, the study “Glucose Metabolism in the Insula and Cingulate Is Affected by Systemic Inflammation in Humans” measures, for the first time, brain activity when subjects were at rest.
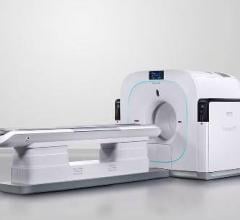
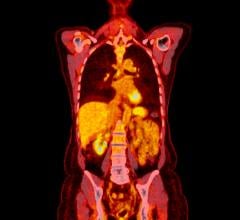
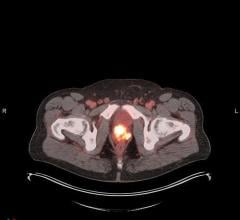
“In the study we used F-18 fluorodeoxyglucose (FDG) positron emission tomography (PET), which can accurately measure glucose metabolism in the brain, to determine which brain regions responded to systemic inflammation. Since the subjects were at rest, the changes we observed in the brain can only attributed to systemic inflammation,” said Jonas Hannestad, M.D., Ph.D., lead author of the article.
In the study, nine healthy individuals received a double-blind endotoxin (which elicits systemic inflammation and mild depressive symptoms such as fatigue and reduced social interest) and placebo on different days. After administration, F-18 FDG PET was used to measure the differences in the cerebral metabolic rate of glucose in the insula, cingulate and amygdala regions of the brain. Behavior changes were also primarily assessed on the Montgomery-Asberg Depression Rating Scale (MADRS).
A statistical analysis of the results showed that endotoxin administration was associated with a higher normalized glucose metabolism (NMG) in the insula and lower NMG in the cingulate compared to the placebo; there was no significant difference in the NMG in the amygdala. Seven of nine subjects had an increase in NMG in the insula and a decrease in NMG in the cingulate, and all nine subjects had a decrease in NMG in the right anterior cingulate, suggesting that systemic inflammation induces fundamental physiologic changes in regional brain glucose metabolism. In addition, the MADRS increased for each subject after endotoxin administration, whereas no significant change was noted with the placebo.
Most researchers agree that depression is not a homogeneous disease, but rather that there are multiple mechanisms that can lead to similar symptoms. “If we can show that a subtype of depression is caused in part by inflammation, we can test the ability of treatments that reduce inflammation in only patients in whom we believe inflammation plays a role,” said Hannestad. “In the future, I expect that researchers in this field will be able to develop more precise PET measures that can be used to distinguish between, for instance, a person with ‘inflammatory depression’ and a person with another kind of depression. PET could then be used as diagnostic biomarker to separate subtypes of depression and as a therapeutic biomarker to detect the response to treatment.”
Nearly 17 percent of adults experience depression at some point in their lifetime, with 30.4 percent of cases classified as severe, according to the U.S. National Institute of Mental Health. Fifty-seven percent of adults with depression report receiving treatment in the past 12 months, although 37.8 percent receive minimally adequate treatment.
For more information: http://jnm.snmjournals.org

 July 30, 2024
July 30, 2024