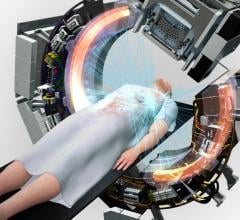
Varian's On-Board Imager.
November 18, 2009 - Intensity-modulated radiotherapy (IMRT) and image-guided radiotherapy (IGRT) are enabling radiation oncologists to enhance post-treatment health-related quality of life for patients with head and neck cancer, according to clinical studies presented an educational session for radiotherapy professionals.
At the annual meeting of the American Society for Radiation Oncology (ASTRO) in Chicago earlier this month, Avraham Eisbruch, M.D., professor at the University of Michigan, discussed how careful implementation of IMRT in the treatment of head and neck cancer can achieve high tumor control rates while minimizing xerostomia, a dry mouth condition that occurs when salivary glands are damaged.
Citing a new report summarizing results from RTOG 0022, a multi-institutional study comparing IMRT with earlier forms of treatment for head and neck cancer, Dr. Eisbruch said that IMRT for head and neck cancer achieved important goals in reducing treatment toxicity, notably xerostomia, and in yielding a high tumor control rate of 90 percent. (Eisbruch A et al. Multi-Institutional Trial of Accelerated Hypofractionated Intensity-Modulated Radiation Therapy for Early-Stage Oropharyngeal Cancer (RTOG-022). Int. J. Radiation Oncology Biol. Phys., in press, doi:10.1016/j.ijrobp.2009.04.011.)
For patients enrolled in the study and treated with IMRT, only 55 percent experienced Grade 2 or worse xerostomia at six months after treatment, as compared with 84 percent of patients treated with earlier forms of radiotherapy, representing a reduction of 35 percent. For the IMRT group, the percentage of patients with Grade 2 or worse xerostomia decreased steadily, to 25 percent at 12 months and 16 percent at 24 months.
IMRT involves shaping radiotherapy treatment beams so that they deliver a dose pattern that matches the size and shape of a targeted tumor while minimizing exposure of surrounding healthy tissues and organs. This approach has been widely adopted by radiation oncologists for the treatment of diverse forms of cancer. Ongoing clinical studies are now maturing, allowing long term outcomes to be assessed and validating IMRT based on clinical data.
Lei Dong, Ph.D., associate professor of medical physics at the MD Anderson Cancer Center in Houston, Texas, detailed how new image-guidance technologies further enhance the accuracy of IMRT treatments by enabling clinicians to correct for patient set-up uncertainties and anatomical changes over a course of treatment.
Dr. Dong discussed the issue of basing radiotherapy treatment plans on single CT scans taken during treatment simulation. "Internal motion can affect the accuracy of tumor definition if the CT scan is acquired while the patient is swallowing," he said, referencing the study Inter-fractional Movement of the Larynx and Oropharynx during Radiotherapy, which he worked on with colleagues from M. D. Anderson Cancer Center.
According to Dr. Dong, stereoscopic X-ray imaging and volumetric cone-beam CT imaging, two imaging techniques enabled by Varian's On-Board Imager kV imaging device, make it possible to fine-tune patient positioning just prior to each daily treatment. In addition, frequent imaging can alert clinicians to changes in a patient's anatomy over time, so that a new treatment plan can be developed part-way through a course of treatment whenever warranted--a process called adaptive radiotherapy.
"Preliminary studies have shown that combining IGRT and adaptive IMRT replanning can improve the overall quality of the treatment plan and, most importantly, reduce unnecessary doses to normal organs surrounding the tumor, such as the parotid glands and oral cavities," Dr. Dong said in the study Prospective Experience with CT-Guided Adaptive Radiotherapy for Head and Neck Cancer. "Combining IGRT with IMRT creates a powerful tool for high precision radiation therapy."
For more information: www.varian.com


 July 09, 2024
July 09, 2024