October 14, 2011 – Positioning breast cancer patients on their stomachs rather than their backs for radiotherapy could lead to better outcomes, according to a radiation oncologist who was among several clinical experts speaking in front of more than 500 oncology professionals about advances in cancer care at a symposium in Miami Beach, Fla., last week.
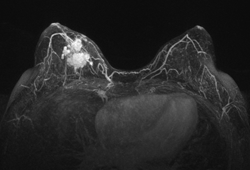
Silvia Formenti, M.D., radiation oncologist at New York University School of Medicine, presented research into the advantages of positioning breast cancer patients on their stomachs (prone) rather than on their backs (supine) during post-lumpectomy radiotherapy. Summarizing trials conducted at NYU, she said that using a prone position for treatment can enable a significant reduction in the volume of lung and heart tissue exposed to radiation for women with breasts of all sizes. "Prone positioning was optimal in sparing the lungs in virtually all right breast cancer cases, and for 85 percent of left breast cancer cases," she said.(1) Formenti also pointed out that research has shown the prone set-up reduces the amount of respiratory motion of the chest wall, which may further enhance the accuracy of targeting during treatment.(2) There is a contraindication, however; the prone set-up appears to be inadequate for breast cancer patients requiring radiotherapy to axillary lymph nodes.(3)
Formenti was among several leading clinicians from major cancer centers in the United States, Italy, and the Netherlands who presented at a clinical forum in Miami last week, sponsored by The Institute for Medical Education, detailing how advances in technology are enabling new approaches in the treatment of lung, liver, breast, rectal and gynecologic cancer. In addition to potentially improving the quality of radiotherapy for breast cancer, researchers are finding that non-invasive radiosurgery can be a viable alternative to surgery in some cases.
Suresh Senan, Ph.D., of VU University Medical Center in Amsterdam, discussed stereotactic ablative radiotherapy (SABR), a form of radiosurgery for tumors in the torso. SABR, which is also sometimes referred to as stereotactic body radiotherapy (SBRT), has shown promise for the treatment of both inoperable and operable stage 1 non-small cell lung cancer (NSCLC), according to Senan. "We are getting excellent tumor control rates, while toxicities of grade 3 or higher are uncommon," Senan said.(4)(5) "Patients largely maintain their pre-treatment levels of pulmonary function."(6)(7)
Beatriz Amendola, M.D., radiation oncologist with Innovative Cancer Institute in South Florida, summarized the results of NSCLC studies from Japan, the United States and Europe, showing that SBRT achieved local tumor control rates between 80 percent and 95 percent at two-three years post-treatment.(8)(4)(5) Researchers from Japan compared five-year overall survival rates for patients treated with surgery versus SBRT by analyzing long-term multi-institutional data. According to Amendola, they found that SBRT "is promising as a radical treatment for operable Stage 1 NSCLC. The survival rate with SBRT is potentially comparable to that of surgery," she said.(8)
Marta Scorsetti, M.D., chief physician at the Humanitas Clinic in Rozzano-Milan, Italy, outlined her institution's early results using “high intensity mode—a very high dose delivery rate available on Varian's TrueBeam platform—in the delivery of SBRT treatments for lung, liver, and abdominal cancers. Summarizing a paper she and her colleagues published recently in Radiation Oncology, she saw Grade 2-3 toxicities among only seven out of 70 patients, with no toxicities greater than Grade 3. The study concludes that high intensity mode SBRT appears to be a feasible approach to treatment for various primary and metastatic lesions in the body.(9)
More than 500 radiation oncology professionals attended the clinical forum, which was supported by an unrestricted educational grant from Varian Medical Systems.
For more information: www.varian.com
(1) Formenti S et al. Results of NYU 05-181: A Prospective Trial to Determine Optimal Position (Prone versus Supine) for Breast Radiotherapy. Int J Radiat Oncol Biol Phys. 2009; 75(3) Supplement, S203-S204.
(2) Morrow NV et al. Intra- and Interfractional Variations for Prone Breast Irradiation: An Indication for Image-Guided Radiotherapy. Int J Radiat Oncol Biol Phys. 2007; 69(3) 910-917.
(3) Huppert N. et al. The role of a prone setup in breast radiation therapy. Frontiers in Oncology. 2011 Oct; Volume 1, doi: 10.3389/fonc.2011.00031.
(4) Timmerman R et al. Stereotactic Body Radiation Therapy for Inoperable Early Stage Lung Cancer. JAMA. 2010;303(11):1070-1076.
(5) Lagerwaard FJ et al. Outcomes of risk-adapted fractionated stereotactic radiotherapy for stage I non-small-cell lung cancer. Int J Radiat Oncol Biol Phys. 2008;70(3):685–692.
(6) Chi A et al., Radiotherapy & Oncology. 2010; 94 (1) 1-11.
(7) van der Voort van Zyp NC et al. Stereotactic body radiotherapy using real-time tumor tracking in octogenarians with non-small cell lung cancer. Lung Cancer. 2010 Sep;69(3):296-301.
(8) Onishi H et al. Stereotactic Body Radiotherapy (SBRT) for Operable Stage I Non–Small-Cell Lung Cancer: Can SBRT Be Comparable to Surgery? J Radiat Oncol Biol Phys. 16 July 2010. Epub ahead of print 10.1016/j.ijrobp.2009.07.1751.
(9) Scorsetti M et al. Feasibility and early clinical assessment of flattening filter free (FFF) based stereotactic body radiotherapy (SBRT) treatments. Radiat Oncol. 2011; 6(113).
SOURCE Varian Medical Systems


 August 09, 2024
August 09, 2024 








