August 29, 2017 — Radioembolization is a radiation therapy method used for liver tumors that are uncurable with surgery or chemotherapy. Thorough development of an individual plan is important for successful treatment. Within the SIRTOP project, the Fraunhofer Institute for Medical Image Computing MEVIS in Bremen, Germany, is developing sophisticated computer algorithms to make therapy planning faster and more precise. The research team will present their initial results at several upcoming conferences.
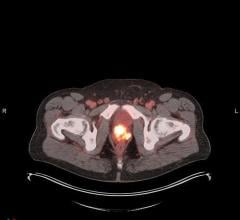
During radioembolization, also known as selective internal radiotherapy (SIRT), tiny glass or resin microspheres are injected into liver arteries using catheters. The microspheres contain radioactive yttrium-90 that irradiates the tissue very intensively in the vicinity of few millimeters. Generally, cancerous lesions receive higher arterial blood supply than healthy liver tissue. As a result, radioactive microspheres accumulate mainly in the tumors. Yttrium-90 has a half-life of 64 hours, so the beads maintain their radioactive effect over several days. They also obstruct the capillary vessels that feed the tumor, significantly reducing its blood and nutrient supply. The combined effects of irradiation and undersupply prevent cancer growth, induce cancer cell death and induce tumor shrinkage.
Thorough treatment planning is an important prerequisite for radioembolization. To damage the tumors maximally, they should receive the highest possible radiation dose in the form of microspheres. At the same time, healthy liver tissue should remain unharmed. In the SIRTOP project (Optimization of Selective Internal Radiation Therapy in the Liver), Fraunhofer MEVIS is developing new software tools, including self-learning algorithms, to support physicians with the therapy planning.
Data from computed tomography (CT) and magnetic resonance imaging (MRI) serve as the basis for planning. These radiological images allow assessing the volume of the patient’s liver and the count, size and locations of tumors in the organ. This basic information helps physicians determine how many radioactive microspheres to inject. Until recently, medical specialists estimated this so-called tumor burden based on the tumor-to-liver volume ratio. Assessing multiple lesions is time-consuming, often lasting more than 15 minutes. “We developed a method that can automatically complete the task with the help of deep learning algorithms,” said project manager Andrea Schenk. “Instead of 15 to 30 minutes, our method only needs an average of less than three minutes to achieve comparable accuracy.”
In April, the MEVIS algorithm took second place among the 14 contestants at the International Symposium on Biomedical Imaging (ISBI 2017) in Melbourne, Australia. The team placed third of 24 participants in the competition of the Medical Image Computing and Computer Assisted Interventions Conference (MICCAI 2017) that will be held in Quebec in September. The goal of both competitions was to identify the tumor dimensions inside the liver as precisely as possible based on predetermined CT datasets.
In addition to developing algorithms for determining tumor burden, SIRTOP tackles another aspect of therapy planning – calculating the optimal radiation dosage for individual patients. In practice, doctors often use a relatively simple method that correlates the values for tumor burden with the patient’s height and weight. MEVIS researchers are developing a more precise approach. Their computer model analyzes the arterial system of the liver and determines which blood vessels supply the tumors. “If we place the injection catheter in those exact arteries or their junctions, we can give the tumor a higher dosage of radiation,” explained Schenk. “This way, we may destroy it more precisely without further impairing the healthy tissue.” The new model does not just help in making global statements about the dose distribution in the entire liver: it also aids observing the dose in different areas of the liver.
MEVIS researchers will present their interim results at the Annual Conference for Biomedical Technology and Three-country Conference for Medical Physics (BMT 2017) in Dresden, Germany, on Sept. 12 and at the annual conference of the Cardiovascular and Interventional Radiological Society of Europe (CIRSE 2017) in Copenhagen, Denmark, Sept. 16-20. Following these conferences, further evaluations of the method are planned using imaging data currently provided by clinicians in Dresden and Yokohama, Japan.
“By the end of the project in autumn 2018, a tool that significantly improves the therapy planning will be available,” said Schenk. Thereafter, the method’s effect on therapy success will be evaluated in clinical studies.
For more information: www.mevis.fraunhofer.de


 August 09, 2024
August 09, 2024