December 23, 2009 – In a new study published in the January issue of Radiology, 42 percent of women eligible for breast cancer screening with MRI declined to undergo the procedure.
“Given that MRI is promoted as a very sensitive test to identify early breast cancer, we were surprised that barely half of women at increased risk for breast cancer would undergo MRI even when offered at no cost,” said Wendie A. Berg, M.D., Ph.D., breast imaging specialist at American Radiology Services, Johns Hopkins – Green Spring Station in Lutherville, Md. “This suggests the need for alternative methods, such as ultrasound, to help screen women at increased risk for breast cancer.”
Some groups of women who are at high risk for breast cancer need to begin screening at a younger age, because they often develop cancer earlier than women at average risk. However, women below age 50 are more likely to have dense breast tissue, which can limit the effectiveness of mammography as a screening tool.
Multicenter trials have shown that MRI enables radiologists to accurately identify tumors missed by mammography and ultrasound. The American Cancer Society recommends that some groups of women with a high risk of developing breast cancer should be screened with MRI in addition to their yearly mammogram beginning at age 30.
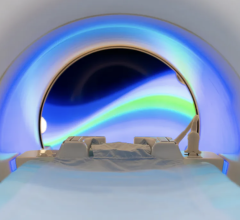
Two factors known to reduce patient acceptance of breast MRI include claustrophobia and the requirement of an intravenous contrast agent. Open MRI causes less anxiety and claustrophobia than closed MRI, but its lower field strength does not allow optimal breast imaging.
As part of the American College of Radiology Imaging Network (ACRIN) 6666 trial, Dr. Berg and colleagues set out to gauge patient acceptance of MRI as a breast screening tool. For the MRI study, 1,215 eligible women at intermediate or high risk for breast cancer enrolled in the ACRIN 6666 trial were offered a contrast-enhanced screening MRI exam. Of those women, only 703 (57.9 percent) agreed to the exam and only 51.6 percent completed the exam per protocol.
The chief reason given for nonparticipation was claustrophobia. One-quarter of the women who refused the exam, or 130 out of 512, cited claustrophobia as the reason. Ninety-three (18 percent) cited time constraints, and 62 (12 percent) cited financial concerns involving insurance. Other reasons for refusal included absence of indication for the exam, lack of interest, medical inability to tolerate MRI, reluctance to receive intravenous injection, fear of further testing or biopsy, MRI scheduling, distance and contrast agent allergies.
Among the 703 who initially agreed to participate, 55 did not undergo the exam for various reasons, including withdrawal of consent, scheduling problems and missed appointments. An additional 21 patients did not complete the exam, had unreadable results or did not meet the protocol deadline. Ultimately, only 627 or 51.6 percent of the eligible women completed a screening MRI. Participation was higher among women with very high lifetime risk of cancer than among women with intermediate risk.
For some women, particularly those at intermediate risk, such as women with extremely dense tissue and many women with a personal history of breast cancer, supplemental screening with breast ultrasound in addition to mammography may represent a viable alternative to screening MRI.
“Screening with ultrasound helps to show small invasive cancers not seen on mammography and can be used to supplement mammography in high-risk women who cannot undergo MRI screening,” Dr. Berg said. “Women who are at increased risk due to intermediate family history or dense breast tissue but do not meet the recommended risk level for MRI can also consider screening with ultrasound in addition to mammography.”
The study is supported by grants from The Avon Foundation and the National Cancer Institute.
For more information: radiology.rsnajnls.org


 July 29, 2024
July 29, 2024