September 20, 2007 - Biopharmaceutical researchers have found a protein in blood they say is linked to all stages of lung cancer but which rarely shows up in the blood of people without the disease.
Testing for this protein might help physicians decide whether smokers or others at high risk for lung cancer should be referred for lung imaging, say investigators, who presented their findings in Atlanta, Georgia at the American Association for Cancer Research's second International Conference on Molecular Diagnostics in Cancer Therapeutic Development.
A diagnostic blood test to screen high-risk individuals for lung cancer could be both practical to use and cost-effective, say investigators from Panacea Pharmaceuticals, Inc., of Gaithersburg, Md.
"A positive test for this protein marker, followed by CT scanning, may help identify individuals with lung cancer at a stage in which treatment is more effective, possibly even curative," said research scientist Mark Semenuk, who is presenting results of a study testing the specificity and sensitivity of the blood test.
Currently, there are no approved blood tests available to help detect lung cancer, which is expected to be diagnosed in 213,000 people in the U.S. this year, and will be responsible for more than 160,000 deaths, according to the National Cancer Institute. Typically, CT scanning or chest x-rays are performed on people who have developed symptoms of lung cancer, but by the time a patient is symptomatic the disease is often well advanced. These two methods are not often used in early screening for potential lung cancer given such issues as price and whether radiological methods are appropriate for routine screening on a large scale."
The protein targeted in the blood test is Human Aspartyl (Asparaginyl) ß-Hydroxylase (HAAH), which Panacea Pharmaceutical researchers say is abnormally expressed on the surface of cancer cells, compared to normal cells, where it resides inside the cell body. HAAH is also found in the serum of individuals with cancer. The protein recognizes cell surface growth factors and modifies them, Semenuk says, pushing the cells into uncontrolled growth. It is likely that increased expression of HAAH is an early step in cancer development, since all stages of lung cancer express roughly the same level of the protein compared to adjacent normal cells.
Thus detection of HAAH in the bloodstream can detect lung cancer before it becomes symptomatic, he says.
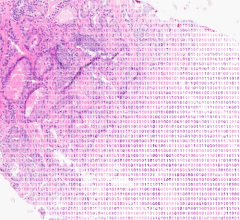
Staining of normal versus cancer cells has found that HAAH is expressed in a wide range of carcinomas, including lung cancer, Semenuk reports. In this study, researchers found that 99 percent of 160 patients who represented all stages and various types of lung cancer, had high levels of HAAH protein in their blood, but only nine percent of 93 non-smokers without lung cancer had a positive HAAH blood test.
In a group of 50 smokers not known to have cancer, four patients had levels of HAAH that were higher than the projected "cut-off" line established between cancer development and no disease, Semenuk says. It is not known, however, whether these four people did eventually develop lung cancer, because the samples were provided for study without access to patient records, and further tests may change that cut-off point, he adds.
For more information: www.aacr.org

 September 07, 2023
September 07, 2023