January 27, 2009 - Children’s Hospital Boston, MA, is offering a new therapy that uses radioiodine labeled metaiodobenzylguanidine (I-131 MIBG) to treat patients with relapsed neuroblastoma, marking the first time this therapy is being used in the New England region.
Neuroblastoma is a cancerous tumor that begins in nerve tissue of infants and very young children, and usually occurs in the abdomen but can occur in other sites near the spine and spread quickly to other areas of the body. It affects roughly 600 children a year in the U.S. and can have a varied clinical presentation – some cases are localized and easy to treat, while more than half of the children have aggressive disease that has spread at diagnosis and is much harder to cure.
Conventional treatments for neuroblastoma include surgery, local radiation and high-dose chemotherapy. “We are always looking for novel ideas and strategies to try to cure relapsed patients whose neuroblastoma is resistant to traditional treatments,” said Suzanne Shusterman, MD, attending physician at Children’s Hospital Boston and Dana-Farber Cancer Institute who oversees the neuroblastoma program. “I-131 MIBG is one of the most effective therapies for children with relapsed neuroblastoma, with a response rate of almost forty percent. While it doesn’t cure, I-131 MIBG can allow patients to gain control of their disease and, in combination with other treatments, bring them closer to being cured.”
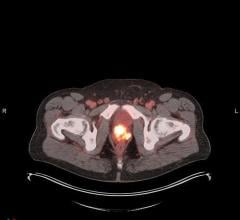
Originally developed as a blood pressure medicine, MIBG is a compound that is selectively absorbed by certain types of nervous tissue, including neuroblastoma cells. For many years it has been used diagnostically to determine where cancerous activity is occurring within the body. More recently, oncologists began using it to deliver targeted radiation to neuroblastoma cells by binding it to a radioactive isotope of iodine (I-131). Once bound together, the radioactive MIBG is administered to a child through an intravenous line (IV) and absorbed by tumor cells, which are killed by the radiation emitted by the radioactive I-131. Children’s is the only center in New England, and just one of a handful in the United States, offering this advanced treatment.
“This treatment is a way of targeting radiation to kill tumors while sparing normal tissues,” said Lisa Diller, M.D., clinical director of Pediatric Oncology at Dana-Farber Cancer Institute and Children’s Hospital Boston. “We are very excited that I-131 MIBG will be an important therapy in eradicating neuroblastoma.”
The actual infusion of I-131 MIBG is a short procedure, lasting approximately one to two hours. Because this treatment involves delivering high doses of radiation, a patient will stay in a specially designed room in the hospital for three to seven days after the infusion. The I-131 MIBG room is a 256 square-foot hospital room located in the stem cell transplant unit on the sixth floor of Children’s Hospital. The room has added protective features to help manage the therapy safely for the benefit of both patients and staff, and has an anteroom where parents may stay to help with the care of their child and be in close proximity throughout the therapy. During the day parents may safely spend time with their child following specific safety procedures designed to protect them as well as the hospital staff.
Compared to chemotherapy, I-131 MIBG is very well tolerated and affords a good quality of life for patients traditionally overwhelmed with hospital visits. The most common side effects are low platelets and low white blood cell counts about a month after receiving the treatment, both of which can be easily managed. Follow up visits to the hospital are also limited, most often taking place six to eight weeks after the date of infusion.
Almost all patients report at least a subjective response to I-131 MIBG. “The nice thing with I-131 MIBG is that most patients, even patients who don’t have a response that we can see by standard imaging techniques, have a decrease in their level of pain and improvement in their quality of life,” continued Shusterman.
S. Ted Treves, M.D., chief of the division of Nuclear Medicine at Children’s, commented, “The availability of this therapy demonstrates a true team effort and commitment from experts in multiple disciplines across the hospital – from pediatric oncology to nursing, child life, nuclear medicine and radiation safety.”
For more information: www.childrenshospital.org


 July 31, 2024
July 31, 2024