May 26, 2016 — Radiation oncologists from across the United States convened on Capitol Hill this week to encourage members of Congress to invest in cancer research with sustainable and predictable funding. Their other goal was to protect patients’ access to high-quality cancer care through value-based physician payment models. The 95 doctors were in Washington for approximately 150 meetings with Congressional leaders from their home districts and states as part of the American Society for Radiation Oncology’s (ASTRO) 13th annual Advocacy Day.
ASTRO members emphasized four priorities as they met with legislators and Congressional staffers: (1) to invest in cancer research with sustainable and predictable funding; to protect patients’ access to quality healthcare by (2) stabilizing Medicare payments while pursuing innovative models of physician reimbursement and by (3) ending physician self-referral abuse; and (4) to preserve funding and residency slots for graduate medical education.
Driven largely by Vice President Joe Biden’s push to accelerate cancer research progress and the launch of the National Cancer Moonshot Initiative, research on treatments and cures for cancer has become a national conversation, and ASTRO members encouraged Congress to ensure radiation oncology is part of that discussion. Radiation therapy has been a safe, effective and powerful method of fighting cancer for more than 100 years, yet federal funding for research in radiation oncology remains well below the level of funding for other therapeutic modalities.
The research community is on the cusp of finding better treatment options for cancer patients, such as combination approaches using radiation therapy to jump-start a patient’s immune system and enhance the effectiveness of immunotherapy. Understanding how and why these combination therapies eliminate cancer cells is critical to matching the right treatments to the right patients, and that understanding necessitates sustained, predictable growth in funding that supports collaboration between the best scientists in far-reaching fields, including radiation therapy.
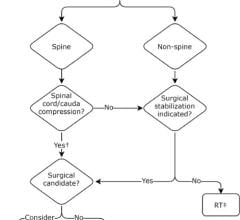
In addition, ASTRO members advocated for support of ASTRO-developed alternative physician payment policies that improve the value of healthcare and protect patient’s access to high-quality cancer care. ASTRO is soliciting public input on an alternative payment model for palliative treatment for bone metastases and will release additional models for public comment.
In the fall of 2015, ASTRO organized a comprehensive response to Medicare payment threats that included obtaining support for radiation oncology against Medicare payment cuts from 207 members of Congress representing both chambers and both major parties. Led by Sens. Richard Burr (R-N.C.) and Debbie Stabenow (D-Mich.), and Reps. Devin Nunes (R-Calif.) and Paul Tonko (D-N.Y.), the support letters called particular attention to the burden that community-based clinics would face by losing the payment stability that is essential to ensure accessible, affordable care for their patients.
Thanks in part to radiation oncology’s Congressional champions, reimbursement reductions in the final 2016 Medicare Physician Fee Schedule (MPFS) were less severe than originally proposed. Moreover, the Patient Access and Medicare Protection Act (S. 2425) passed in December, freezing payment rates for freestanding radiation oncology centers through 2018 at the levels set under the 2016 MPFS and bringing these centers one step closer to payment stability.
Medicare payment stability allows radiation oncology to transition away from the antiquated “fee-for-service” model toward the promise of alternative payment models (APMs) authorized under the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA). APMs incentivize physician participation in performance-based payment models and move the reimbursement structure from a system of volume to one of value. ASTRO members emphasized the potential for specialty medical societies to help lawmakers incorporate robust quality improvement programs into APMs and the Merit-based Incentive Program (MIPS) under MACRA.
“ASTRO’s advocacy efforts since 2009 have prevented more than $500 million in proposed Medicare payment cuts to radiation oncology, and we’ve helped pass legislation that brings some much-needed payment stability to doctors across the discipline through 2018” said ASTRO Chair Bruce D. Minsky, M.D., FASTRO. “In addition to fighting for fair and stable reimbursement, ASTRO is leading the way to develop alternative payment models for radiation oncology that will support the delivery of high value, high quality care for our patients.”
ASTRO also encouraged Congress to protect patients by helping ensure treatment decisions are based on clinical judgment rather than financial gain, through narrowing exceptions in the Ethics in Patient Referrals Act that allow for physician self-referral abuse. Multiple studies, such as 2013 reports published by the Government Accountability Office (GAO) and in the New England Journal of Medicine, have shown that physician self-referral leads to increased utilization of services that may not be medically necessary and poses a potential risk of harm to patients. The Promoting Integrity in Medicare Act of 2016 (HR 5088) introduced by Reps. Jackie Speier (D-Calif.) and Jim McDermott (D-Wash.) would close the loophole in current policy that allows for self-referral abuse, help drive payment and delivery system reform and save an estimated $3.3 billion dollars in unnecessary Medicare spending over the next decade.
A final legislative priority for ASTRO is to preserve funding for graduate medical education by supporting the Training Tomorrow’s Doctors Today Act (HR 4774). The American Cancer Society estimates that more than a million and half people in the United States will be newly diagnosed with cancer this year alone. Coupled with the disproportionate growth projected among the American elderly population, the growing numbers of cancer patients and survivors are creating a steadily increasing demand for medical care – and the physicians to provide that care. An April 2016 report by the Association of American Medical Colleges predicts a shortage of 61,700 to 94,700 physicians in the U.S. by 2025. The Training Tomorrow’s Doctors Today Act would train an additional 3,000 doctors each year for five years, allowing teaching hospitals to expand their residency programs, while concurrently establishing new accountability criteria for these programs.
For more information: www.astro.org


 August 09, 2024
August 09, 2024