Getty Images
August 31, 2022 — A new clinical guideline from the American Society for Radiation Oncology (ASTRO) provides recommendations on the use of radiation therapy to treat patients with isocitrate dehydrogenase (IDH)-mutant grade 2 and grade 3 diffuse glioma. Evidence-based recommendations outline the multidisciplinary planning and delivery techniques to manage this subset of central nervous system (CNS) tumors. The guideline, ASTRO’s first for lower-grade glioma, is published in Practical Radiation Oncology.
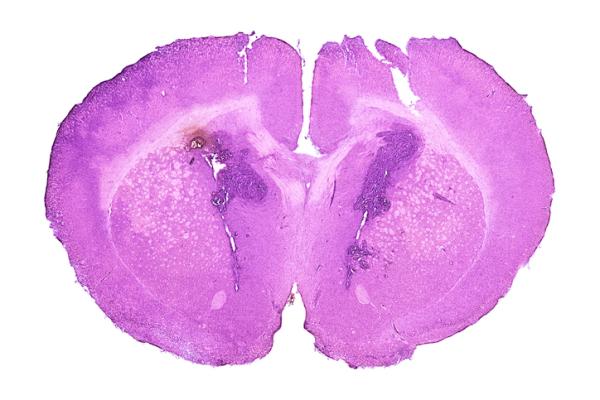
Gliomas are the most common type of primary malignant brain tumors in adults, accounting for nearly 8 in 10 of these tumors. In 2021, the World Health Organization (WHO) reclassified gliomas to reflect the discovery of new biomarkers, including mutations to the genes that encode isocitrate dehydrogenase (IDH) enzymes. IDH mutations occur in 70-80% of patients with lower-grade diffuse gliomas, and patients with IDH mutations tend to have longer survival than patients without them.
The change in WHO tumor grading raised questions about how best to treat patients who fell into the new classifications, explained Helen A. Shih, MD, MPH, Chair of the guideline task force, Director of the CNS & Eye Service in the Department of Radiation Oncology at Massachusetts General Hospital (MGH) and Medical Director of the MGH Proton Therapy Centers in Boston. “For patients diagnosed with low-grade glioma, clinical trials show improved survival outcomes with a variety of treatment approaches. The heterogeneity of patient cohorts in these trials and the use of a now-outdated tumor grading system also can make it difficult to draw conclusions for patient care without clear guidance based on the new WHO classification,” said Dr. Shih.
Studies on U.S. cancer care patterns show wide variation in the use of radiation therapy for patients with low-grade glioma, perhaps due to the lack of definitive overall survival benefit in randomized trials and few central recommendations, said Lia M. Halasz, MD, Vice Chair of the guideline task force, as well as Co-Director of the Alvord Brain Tumor Center and Director of the Radiation Oncology Residency Program at the University of Washington in Seattle. “We developed this guideline to help providers determine the best multidisciplinary management approaches for their patients, taking into account the various options available and implications for long-term outcomes,” said Dr. Halasz.
Recommendations in the guideline address the indications and optimal timing, as well as planning and delivery techniques, for radiation therapy in adult patients with IDH-mutant, WHO grade 2 and grade 3 glioma, including oligodendroglioma and astrocytoma. The guideline also addresses clinical management of adverse effects and includes an algorithm that summarizes the treatment paths. Key recommendations are as follows:
- Generally, close observation after surgery is recommended for patients diagnosed with lower-risk disease, while adjuvant therapy is recommended for patients with any features of higher-risk disease. Features of favorable and poor prognoses, such as resection extent and patient age, are detailed in the guideline.
- Higher-risk disease: Early adjuvant therapy involving radiation therapy with sequential or concurrent/sequential chemotherapy following surgical resection is conditionally recommended for patients with grade 2, IDH-mutant oligodendroglioma (1p/19q codeleted) or astrocytoma, and any features of high-risk disease. It is strongly recommended for patients with WHO grade 3, IDH-mutant oligodendroglioma (1p/19q codeleted) or astrocytoma, with any extent of surgery.
- Lower-risk disease: Close surveillance involving magnetic resource imaging (MRI) and clinical examination every six months following surgical resection is strongly recommended for patients with oligodendroglioma, WHO grade 2, IDH-mutant, 1p/19q codeleted who have more favorable disease prognosis. It is conditionally recommended for patients with grade 2, IDH-mutant astrocytoma and more favorable prognosis.
- Recommendations outline optimal radiation dosing, treatment planning and delivery techniques based on tumor histology and grade. Use of the advanced radiation therapy technique intensity modulated radiation therapy, inclusive of volumetric modulated arc therapy, is recommended to mitigate long-term side effects and preserve patients’ quality of life.
- The guideline also addresses survivorship care, with multidisciplinary approaches to assess and manage treatment-related side effects, and it emphasizes the importance of lifelong surveillance to detect recurrences and late side effects for patients diagnosed with these tumors.
About the Guideline
The guideline was based on a systematic literature review of articles published through July 2020. The multidisciplinary task force of subject matter experts included radiation oncologists, neuro-oncologists, a neurosurgeon, a neuropathologist, a radiation oncology resident and a patient representative. The task force included representatives from the American Association of Neurological Surgeons/Congress of Neurological Surgeons (AANS/CNS), the American Association of Neuropathologists (AAN), the American Society of Clinical Oncology (ASCO) and the Society of Neuro-Oncology (SNO). The guideline was endorsed by the Canadian Association of Radiation Oncology (CARO), the European Society for Radiotherapy and Oncology (ESTRO), the Royal Australian and New Zealand College of Radiologists (RANZCR) and SNO.
ASTRO's clinical guidelines are intended as tools to promote appropriately individualized, shared decision-making between physicians and patients. None should be construed as strict or superseding the appropriately informed and considered judgments of individual physicians and patients.
For more information: www.astro.org


 August 09, 2024
August 09, 2024 








