September 8, 2009 - Americans recognize the value of medical imaging as a critical component of high-quality healthcare, according to an online survey of 4,426 voters conducted September 4 - 8, 2009, by Zogby International and commissioned by Powell Tate.
Specifically, 71 percent of the surveyed voters oppose making further Medicare cuts to advanced imaging tests and screenings, such as MRIs and CT scans, as a means to pay for health care reform, the Access to Medical Imaging Coalition (AMIC), a coalition of physician, patient and imaging manufacturer groups, said today.
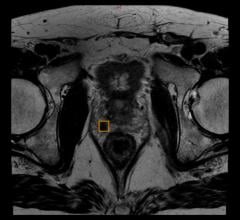
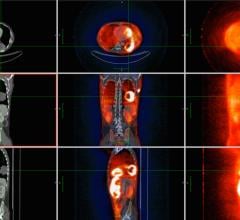
In the online survey, 78 percent of respondents said that Congress’s proposed cuts to medical imaging services, including MRIs, CTs and PET scans, will have a significant impact on physicians’ ability to detect diseases – such as heart disease and cancer – at their earliest stages. Moreover, 66 percent said that President Obama should urge Congress to reject these additional medical imaging cuts when he addresses lawmakers tomorrow.
“Medicare cuts to diagnostic imaging are counter productive to health care reform,” said Tim Trysla, executive director of AMIC. “Early detection saves lives and money and eliminating physicians’ ability to use advanced diagnostic imaging tools will just end up costing Medicare more money and patients’ health will suffer. With nearly 8 out of 10 voters saying that if Congress cuts Medicare spending for medical imaging, early detection will be compromised, it’s clear that the American public understand how important imaging is to health care reform. Now is the time for Congress and the Administration to listen to voters by rejecting deep Medicare cuts to diagnostic imaging services.”
“This survey data confirms what colon cancer patients across the country have been telling us for months,” said Andrew Spiegel, CEO of the Colon Cancer Alliance. “They want the President to stand up for disease prevention and early detection by rejecting further Medicare cuts to life-saving diagnostic imaging.”
AMIC opposes proposals put forth by the Senate Finance Committee and the Obama administration that would limit Medicare patients’ access to diagnostic tests by dramatically increasing the utilization rate assumption for advanced imaging equipment from 50 percent to 90 percent, and by reducing payments for single-session imaging on contiguous body parts by 25 percent. Provisions in the House Tri-Committee’s bill that propose increasing the utilization rate assumption to 75 percent would have a similar effect. If made, these changes to the Medicare reimbursement formula will result in further deep and arbitrary Medicare cuts for imaging and will force imaging centers – foremost those that treat patients in rural America – to close, pull back services or stockpile patients.
“The advanced diagnostic imaging proposals put forth by the Obama administration and the Senate Finance Committee, as well as those in the Tri-Committee’s bill will undoubtedly affect patient access to life-saving services,” said Trysla. Data shows that that imaging equipment in rural regions of the country operates only 48 percent of the time an office is open for business, while equipment in non-rural areas operates just 56 percent of the time. Neither rural nor urban non-hospital diagnostic imaging providers operate equipment at rates anywhere near the levels that are being recommended. This means that setting payment rates using a utilization assumption of 90, or even 75 percent, will cut reimbursements too far and impair access to diagnostic imaging services, ultimately resulting in patients’ delaying or forgoing life-and-cost savings imaging procedures.
“It’s important to keep in mind that payments for diagnostic imaging services were already severely reduced by the Deficit Reduction Act of 2005,” added Trysla. “Another deep and arbitrary cut on top of those rippling through the system now will devastate beneficiaries’ access to services.”
The Deficit Reduction Act of 2005 (DRA) resulted in $1.64 billion in Medicare cuts to advanced imaging in 2007 alone, the first year cuts were implemented—an amount that was three times larger than what Congress intended and the Congressional Budget Office had estimated. The GAO also found that utilization of advanced imaging services has already slowed significantly as a result of the DRA, suggesting that further cuts could go too far and endanger the availability of these services.
Additionally, an analysis of Medicare claims data by The Moran Company shows that from 2006 to 2007, post-DRA, reimbursements for advanced imaging (CT, MR, Nuclear Medicine and PET) fell by 19.2 percent and the volume of these services grew by a modest 1.9 percent.
Rather than proposing utilization rate increases, the medical imaging community supports sensible reform efforts such as appropriateness criteria, accreditation and physician feedback systems to reduce costs and ensure proper utilization of imaging and radiation therapy, without compromising patient access. These measures, if adopted, will ensure that patients have access to high quality care and can receive the right scan at the right time. Moreover, AMIC recommends that Congress defer any changes to the advanced imaging utilization factor until existing data on utilization and patient access are analyzed. This data-driven approach to policy making will ensure that Congress is successful in balancing its goals of high quality, efficient delivery of care, improved access, and lower costs.
For more information: www.rightscanrighttime.org


 July 02, 2024
July 02, 2024