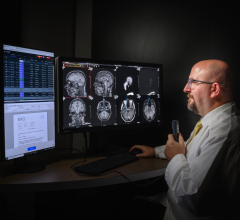
Mark Leavitt, M.D., Ph.D., is the chairman of the Certification Commission for Healthcare Information Technology (CCHIT)
There is a lot of talk about the American Recovery and Reinvestment Act of 2009 (ARRA) and the $19 billion earmarked for IT incentives, but little has been said about how it will impact radiology and radiation oncology IT. One of the leading barriers to faster EHR adoption is cost, a factor the new bill aims to address by injecting the necessary revenue to build an EHR highway. The ARRA states that it is designed to provide funds for hospitals and physicians “to encourage adoption of certified electronic health records (EHR)” by 2011. Of the total package, $17 billion will provide incentive payments via Medicare and Medicaid and $2 billion will go to grants and loans for those who adopt the technology. To qualify for the incentives, physicians and hospitals must use the EHRs in a "meaningful way.” How can radiology and radiation oncology IT contribute to an EHR in a “meaningful way”? According to Mark Leavitt, M.D., Ph.D., chairman of the Certification Commission for Healthcare Information Technology (CCHIT), as long as a physician is using the system to transfer clinically relevant information, such as electronic images and clinical data, “that proves you have an electronic health record.” But first, in order to receive incentives for an EHR, the system must be certified by CCHIT. “Under the AARA, billions of dollars in public funds are being invested in health IT, with certification as a key mechanism to ensure that the electronic health records (EHRs) adopted will deliver the promised benefits in quality, safety and efficiency,” said Dr. Leavitt. Dr. Leavitt spoke with Imaging Technology News (ITN) about the impact the bill will have on EHR adoption and how it will impact radiology and radiation oncology IT. ITN: Can you break down the net investment of the funds from the ARRA? Dr. Leavitt: There are two parts to the funding from the ARRA. The big part goes to Medicare and Medicaid and that is for certified EHRs and for using the certified EHRs in a meaningful way. When the law talks about providers and physicians, it excludes hospital-based physicians. According to the Congressional Budget Office (CBO), which scored it, the macro calculations is that it is a gross amount of $34 billion in incentives total going out and, with a calculated savings from reduced duplication of about half that, net public investment is at about $17 billion – that is the net additional monies allocated. The other part of the funding is $2 billion that goes to ONC and comes out in a variety of programs to support health information exchange, loans and grants for health information technology and education or extension centers. Those in general do not go to individual providers. ITN: How will radiology and radiation oncology groups already using EHRs benefit? Dr. Leavitt: The HHS will create the details of the qualifications in a rule making process. The incentives are for hospitals and professionals. On incentives for professionals, it says it does not apply to hospital-based professionals. Some radiologists are hospital based or other ones are not – so they differ depending on the structure of their practice. The one’s that are hospital-based, that doesn’t mean they won’t benefit because their hospitals will end up with new systems and technology. The hospital benefit will be substantial. ITN: You said: The electronic health records will deliver the promised benefits in quality, safety, and efficiency. Can you quantify the projected improvements in those areas? Dr. Leavitt: It’s very hard to quantify, so it has to be a qualitative discussion. In terms of quality, the bill talks about meaningful use – there are two elements to getting this incentive. One is you must have certified EHR technology, and second you have to be a meaningful user of that technology. The EHRs have to be sending and receiving information electronically, and the EHR has to be reporting on quality measures. The details of how to prove that have to be developed by HHS. That is where you are going to see the expected benchmarks. If you look at the pay-for-performance programs that is a good model to look at. They typically offer an incentive the first year for adopting the technology, the second year for measuring quality – what is the percentage of patients who get this treatment in this many days. Then the third year they expect improvement in quality – can you do a 10 percent year-over-year improvement benchmark, for example. ITN: How long will it take a physician office to see a ROI once it implements an EHR? Dr. Leavitt: In a physician office it depends on if you are currently using dictation and transcription to generate the records. If they are using dictation and transcription and they are able to reduce that because of an electronic healthcare record, then they can often get an ROI in a year or two because the transcription costs can be $10,000 or $15,000 per doctor per year. That is one of the bigger potential savings. In a hospital, the way you’re saving is through shorter lengths of stay because you didn’t have someone waiting while a result was moved around in a cart and pasted on a chart. If you get the results instantly with an EHR, you will save money. ITN: CCHIT announced the expansion of its roadmap for its health information technology (HIT) certification activities. What is the objective of this expansion? Dr. Leavitt: The HHS currently recognizes us and the bill says the national coordinator shall recognize a program for certification in EHR technology, and we are the only recognized program. The expansion comes about because as certification’s impact has increased, the interest has grown from beyond the original three areas of the contract. We had a contract with HHS to certify ambulatory EHRs, inpatient EHRs and health information exchanges. There was a lot of demand from other specialties for us to bring certification to those areas. So we started expanding in 2007 and in 2008 we launched first expansion round. We expanded to the emergency department, we added child health, cardiovascular medicine, an enterprise certification. This summer we will be adding personal health records and prescribing. So our roadmap is telling you where we are going beyond that. This new law is going to have an enormous affect on everything, so we are remaining flexible. We might have to add more areas or substitute systems because everyone wants certified systems to qualify for the incentives in the recovery act. This includes anyone buying or selling an EHR. The areas we will develop and launch next year would be behavioral health as an add-on capability for EHRs, dermatology, advanced certifications in interoperability and in quality measurement, and certifying EHRs in the long-term care spectrum. In 2011, we hope to launch the eye care spectrum, which is ophthalmology and optometry, advanced certifications in security and clinical decision support and also oncology. There is a crossover between oncology and radiation oncology in our roadmap being part of oncology. The reason we put oncology in 2011 and not 2010 is that is big and complicated. We’ll be doing some research on the needs in the next year and we will need to figure out how radiation therapy fits with oncology. Our EHRs for oncology are different from ambulatory. We have to understand how people are buying this. We need to figure out how radiation therapy fits with oncology. Is it done by radiologists or oncologists? The EHRs used by radiation oncologists are fundamentally different from those used by ambulatory oncologists. We have to understand the field before we start certifying because the certification has to match the marketplace – the way people are buying systems. ITN: CCHIT has several work groups such as Ambulatory EHR, Cardiovascular Medicine and Emergency Department EHR. For radiology, does the PACS filter in to each one of these types of EHRs? Dr. Leavitt: If PACS is a departmental system that is separate from the core EHR, then it wouldn’t qualify for the incentive, but if it is defined as a module as part of an EHR, then it would. That is one of the things we have to sort out as we move forward. We still need to research this. In order to get funding from the bill, you just have to be using the certified EHR technology in order to get the incentive payment. You don’t have to, for example, wait to buy it this year; you have to be a user of it this year to get the payment. Or if you already own it, and you prove it certified and used in a meaningful way, then you qualify for the incentives. For example, if a hospital has gone all digital, whether they got an entire system or modules. That system should be certified, yet the departmental systems would not have to be to meet the criteria of meaningful use. We won’t need to certify every system. There may be a subsystem within a PACS – a module that does something special - that we wouldn’t have to certify. It’s really the fact that they have clinical information and that they are using it. These modules will have a valuable role. For example, if a patient’s in an accident across the country and they take a CT of the head and see an abnormality and need to know if that’s new. They need to see a prior CT scan in different location. So, if one hospital can send that information, that’s an exchange of information, and that hospital should get an incentive. It doesn’t matter if you bought the EHR first or PACS or if it came integrated. The end result is you have mastery over the electronic images; you can access them and send them where they need to go. That proves you have an electronic health record. The goal is to make this information more portable. ITN: How widely will the stimulus package drive penetration of EHRs in U.S. hospitals? Dr. Leavitt: The CBO has estimated what it will do in penetration in 2015. We know the penetration of EHRs in U.S. hospitals and only a very small percent are using all of the functionality of electronic health records. The majority is on their way, and almost none are exchanging information outside of the walls of the hospital. ITN: What are some factors contributing to the fact that such a low percentage of U.S. hospitals have adopted EHRs? Dr. Leavitt: Because there has not been a requirement or an incentive to do it. Competition amongst different healthcare records has contributed to them not distributing information, and that has got to change. They need to compete on quality and not on how well they can lock up information. That is why health information exchange is one of the requirements because competing and monopolizing information is out of bounds. Reference: DesRoches, Catherine M., et al. Electronic Health Records in Ambulatory Care — A National Survey of Physicians. NEJM. Volume 359:50-60. July 3, 2008.


 February 03, 2025
February 03, 2025