Not too long ago, the capability of precisely directing and guiding a potent beam of radiation to eradicate a cancerous tumor without harming the healthy tissue around it was a pipe dream. Fodder for the imagination and science fiction.
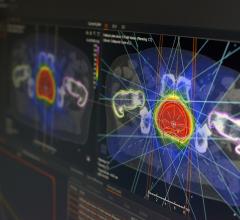
But the advent of treatment planning software changed all that, ushering in a new generation of effective cancer treatments and therapies, such as intensity-modulated and image-guided radiation therapy (IMRT and IGRT, respectively) and even adaptive radiotherapy, along with a variety of accompanying imaging modalities.
With all the improvements that have debuted within the last decade and incorporated into radiation oncology it might be difficult to fathom where treatment planning software developments are headed next. So Outpatient Care Technology set out to explore what the next-generation treatment planning software applications will look like and how their function and role in clinical, financial and operational performance will be enhanced through technological development. OPCT Editor Rick Dana Barlow asked key executives at the leading treatment planning software manufacturers to briefly share their insights on the technological progression of treatment planning software products for outpatient care facilities. In the April/May 2006 edition of OPCT, we heard from three of the thought leaders in this segment. Here, we learn from five more.
With the growing popularity in using radiation oncology to combat cancer, what do you foresee as the next big development in treatment planning software (TPS) applications used to ensure accuracy and proper functionality? Why? How do you envision this next-generation TPS functioning (particularly if it’s different)? Why does this new version represent an advancement over current versions? What additional capabilities and features will be available to enhance patient care, particularly in the outpatient setting? If you could design and program the most futuristic TPS application what features would it include? Do you foresee any of these features being valuable to end- users? Finally, how realistic is it to expect cost-conscious outpatient care facilities to use it?
Randy Hemingway, vice president, sales and marketing, PerMedics Inc., San Bernardino, CA
Treatment planning has made many advances since my therapy training in 1978. As a Certified Medical Dosimetrist (CMD), my interest in treatment planning evolution has been foremost. Odyssey Treatment Planning has taken the steps to be the most advanced solution in the market today and into the future.
Radiation oncology is advancing with improved outcomes through the use of IMRT, radiosurgery and proton therapy. Through these modalities we have become more aware of the problem of patient and organ motion. Many solutions are under investigation to solve this issue, with the initiation of the NIH 4D Tools grants. Ultimately, we know that the relationship of motion, dose and delivery require a form of adaptive therapy planning. Odyssey has been working on these issues, utilizing the most comprehensive solution for these combined modalities, as well as interfacing to multiple patient tracking and imaging solutions.
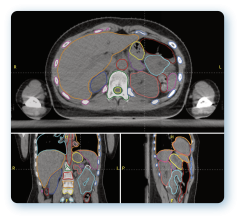
Smaller fields and minimal margins minimize toxicity to the patient. In treatment of early stage lung cancer, we know that with high dose/smaller fields local control is possible. Lung lesions travel in all six directions during breathing as well as possible deformation. [Four-dimensional] CT scanners are allowing us to bin the image study-sets for use in planning to enable modeling of the lesion. The problem becomes the ability to handle these studies in a planning system, when more than 1,000 images must be delineated (contoured). Automatic segmentation tools become immensely important.
High-dose fractionation is becoming more common to many tumor sites. Early stage brain, lung, liver and breast are just a few. This has been recognized by the radiotherapy community and rewarded by higher reimbursement, through image guidance, stereotactic radiosurgery and 6-D robotics.
PBI (Partial Breast Irradiation) is a technique of using hyper-fractionation (five days, two fractions per day at around 400cGy per fraction) for early stage breast cancer. Currently under RTOG protocol, the results thus far appear excellent. The requirement for this site as well as many radiosurgical sites (both intracranial and extracranial) is fixation of the patient, tracking of the patient’s surface, image guidance of the site through planar KV registration or cone-beam reconstruction, and ultimately, a correlation of these solutions.
Mark Russell, president, RAHD Oncology Products, St. Louis, MO
There are two arenas affecting the growing popularity of radiation oncology. One is certainly the technology allowing us to escalate dose; improving cure rate. The other is our ability to discriminate between the tumor and normal tissue, allowing us to spare dose to normal tissues and improve the tolerance to treatment and quality of life. To best understand where development can help the clinician, one must look at the factors to be considered in answering the big question for both of these initiatives: ‘Where’s the cancer?’ Improvements in imaging will continue to be a force that will drive the next generation of cancer therapy development.
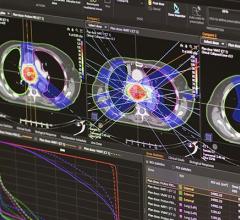
My prediction is that the next-generation 5-D imaging tools (three geometric axis, modality and time factors – all occupying the same geometric volume space), will dramatically improve the ability to discriminate between cancerous and normal tissue. The time factor will probably be the factor that is most evident in the planning tools. Image-guided therapy, by definition, brings an image into play at the time of therapy delivery. Improved tools in imaging will continue to enhance the options for image guidance. Capture of a treatment condition image will then beg the assessment of composite delivered dose, and provide for the ‘delivered’ DVH being used in the continuation of therapy decisions.
At some point in this evolution we will depend less on immobilization and more on the image guidance for accuracy in delivery. The elements that will make this possible are deformable warp fusion tools (to assemble a patient image data resource occupying a common space-coordinate volume, computer-guided region of interest (ROI) and structure segmentation, real-time accessibility and real-time dose calculation.
Diagnosis and staging work-up will begin the build of a volumetric, multimodality, patient-specific, image data resource, occupying a common space and coordinate system that is time discriminatory. Structures and ROIs will be defined, in part, by computer-assisted tools. The initial dose calculation will be derived from inverse optimization or intuitive forward planning applications. Dose evaluation will be available for nearly instantaneous review. Image-guided resources will allow the accumulation of delivered dose to be forward summed and be included in the quality assessment of the treatment process.
The applications will be server-based apps with Wi-Max distribution to allow the technology to follow the clinician instead of requiring the clinician to go to the technology.
To date, our resource for evaluating dose has largely been one-off assessment – if the A = B, and A = C, than A must equal C. Mathematically this is a good expression, but in real time we know that time and reproducibility are not our friends. A system that will help us understand dose in the context of what was delivered (as confirmed by image guidance) will help us reduce the uncertainty of treating the cancer and sparing normal tissue.
Distributed applications have already been mentioned but desire recognition again. The generation of tools that have emerged in the last five years provides us with a great deal of sophistication. Today our problem is more about having those tools available conveniently and in a way where coordinating the input from multiple professionals will improve a busy clinical schedule. Time and efficiency can be greatly improved with broad availability of these tools.
Better planning with electron beams will be in the next-generation planning systems. We will be better able to plan and deliver electron beam contributions with improved accuracy, more efficiency and NO cones. We will be able to deliver electrons in the isocentric model.
[The most futuristic treatment planning software application] would start by accessing a comprehensive data resource of patient image information – and place all that data in the same space-coordinate system. Tumor and structure definition would take place using the most appropriate image source for the task and be reviewable in time perspective (i.e., presurgery images available for post surgery treatment decisions – tumor bed information). Computer tools would create rules-based planning volumes. Forward planning tools will be greatly improved and include multiple modalities. Inverse and optimization tools will be fast and shapeable as the plan matures.
The value will simply be a better plan, more comfortable immobilization and greater precision in delivery. The cancer population as a whole will benefit from a marked increase in participation in treatment protocol evaluation.
Improvements in efficiency will far outweigh the cost – particularly when foundation technology obsolescence (aging computers) will make it prudent to replace hardware. Outpatient care facilities are going to become much more cognizant of the need to maintain database integrity fail-safe technology.
John Nguyen, president and CEO, Prowess Inc., Chico, CA
The incorporation of new image guidance technologies in treatment planning will be the next challenge for radiation therapy. This will include the ability to quickly and automatically re-plan a patient’s radiation therapy based on images acquired on the day of treatment, thus eliminating interfraction treatment errors. Looking forward, we also see the use of 4-D images for minimizing the effect of intrafraction organ motion and optimization of treatments based on functional imaging. As geometric accuracy improves, the pressure for dosimetric accuracy will continue.
The speed and accuracy of dose calculation will continue to be enhanced by medical physics research and advances in computer technology. For example, current advances in computer design, such as multithreading and dual core processing can allow us to run streams of calculations simultaneously, significantly reducing optimization times. The Prowess Panther treatment planning system is taking advantage of these leaps in technology. We are working to integrate advanced IGRT into the Prowess treatment planning system.
[The next-generation treatment planning software] will be faster, easier to use and more accurate. Dose calculation will be in real time and planning will be part of the image guidance system. Just as with IMRT, these IGRT functions help move radiation therapy to the next level. With the application of these technologies, treatment accuracy and effectiveness will be moved forward significantly, increasing beneficial outcomes for patients.
Overall patient treatment schedules in the future will be shorter, due to the increased effectiveness brought on by ‘just-in-time’ planning, thus helping to ease workloads for outpatient radiation therapy staff. The resulting efficiencies will no doubt be attractive for cost-conscious outpatient care facilities. At Prowess, we believe that all clinical software products must be easy to use, and should be cost effective. We want to have the best functionality and offer the best value for our customers so that all clinics can benefit by offering better care to their patients.
Rob Hill, vice president, engineering, NOMOS Radiation Oncology Division, North American Scientific Inc., Chatsworth, CA
We see a greater degree of integration between imaging systems in the treatment room and the treatment planning process. These imaging systems will enable new treatment planning workflows which will increase the precision with which tumors can be targeted. Dose distributions will be hand-tailored by the physician in real time. Dose calculation algorithms will become more and more accurate. Real-time QA will be conducted as part of each patient treatment. These advances will enable development of highly accurate correlations between biological outcome and daily dose delivered.
The workflow will be highly optimized to provide users with the highest benefit for the amount of time spent. The degree of integration between imaging, planning and delivery will increase.
Current treatment planning systems are not optimized for physician workflow, do not take into account imaging available only at treatment time, and have dose calculations whose accuracy is limited under certain circumstances.
Mark Broeders, director of marketing, Resonant Medical Inc., Montreal, Quebec, Canada
Effective treatment planning is predicated on accurately defining the patient anatomy and especially the target volume. Advances in commercial planning systems now support Monte Carlo dose calculation and inverse planning for IMRT. However, these improvements are meaningless if the wrong target has been identified. Cost-effective imaging solutions, like the Restitu 3D ultrasound system, can complement CT imaging to provide superior soft tissue visualization that is required to elevate treatment planning to the next level.
Treatment planning software will continue to play an important role in the evolution of treatment planning. However, to achieve a high-quality output from the planning system, high-quality input in the form of multimodality imaging is necessary.
Restitu represents a new generation of ultrasound image guidance. It is the only system that provides access to ultrasound in the CT room that is automatically or implicitly registered to the CT data making CT-Ultrasound image fusion a reality. As we have seen the sizable increase in CT-PET devices, it is reasonable to believe that CT-Ultrasound image fusion will also experience rapid market adoption.
Feature | June 22, 2006
Last of Two Parts

 June 19, 2024
June 19, 2024