Contouring dose with pinpoint, multidimensional accuracy, targeting a tumor without damaging surrounding tissue and destroying a tumor in one radiation session is still a lofty goal in radiation therapy, and rarely attainable. For years, radiation oncologists and physicists have longed for technology to match their need for imaging and radiation delivery methods that hit all of these objectives.
With the advent of stereotactic body radiation therapy (SBRT), the imaging community might finally have a tool that provides maximum benefit for physicians and patients. Why is SBRT the technology of the future in the field of radiotherapy? What systems exist, and what must be done before widespread adoption in the field? As more studies demonstrate the improved success of using SBRT over conventional methods such as IMRT or IGRT, it becomes clearer that this novel technique may become the treatment of choice in radiation therapy’s near future.
Targeting hard to reach tumors
Radiation therapy has evolved as a delicate balance between delivering the right dose and not damaging surrounding healthy tissue. With conventional external beam radiation therapy, a significant portion of surrounding normal tissue also receives dose to avoid missing the tumor or lesion. This inescapable fact of radiation therapy is due primarily to technical limitations, including the inability to target precisely with existing imaging and radiation delivery methods. Add to that the normal movements of organs and difficulties in patient positioning, and typical radiotherapy could help but also hurt the patient.
More recent radiosurgery methods have attempted to increase precision and remove dosing of healthy tissue. New procedures deliver large radiation doses to tumors and other targets in single or small numbers of sessions, ideally without harming the surrounding healthy tissue. In order to do this companies and tools have experimented with increased radiation delivery speed, dose sculpting and enhanced imaging capabilities. But for the most part, there has not been an option that has included all of the above.
With SBRT, the imaging community is seeing this advance come to life. Stereotactic radiosurgery and radiotherapy have been successfully used for intracranial, orbital and base-of-skull tumors to accurately locate and dose tumors in three-dimensional space. Like these techniques, SBRT involves patient immobilization and image-guided radiation therapy (IGRT). As a subspecialty of IGRT, SBRT enables delivery of extremely precise high doses of radiation to malignant or benign tumors that are small, may be hard to reach and are located typically in the head or neck, lung, liver, in various abdominal sites and the prostate. With tighter margins, less normal tissue is affected so there are fewer side effects for patients. Plus, fewer treatment sessions are required to deliver the same total amount of radiation.
The proof is in the imaging
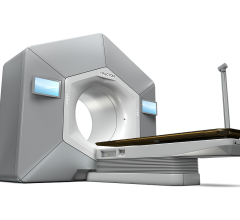
Extending this technique to the body required advances in imaging, radiation delivery and patient placement. New SBRT systems that image, localize and sculpt radiation for small to moderate-sized tumors in the body is now available.
“The advances occurring in radiotherapy are unprecedented,” said Cal Huntzinger, manager of marketing and engineering, surgical sciences, Varian Medical Systems. “With our new SBRT systems, we have the ability to identify targets in ways we never could before, driven by the power of functional images combined with structural images. Oncologists and referring physicians can visualize exactly what they’re trying to treat without guessing. During treatment, physicians can sculpt the dose in ways that were unheard of just years ago.”
The key to the new capabilities of SBRT is significant advancements in imaging. While in the past radiotherapy and radiosurgery primarily used CT scans for target identification and treatment, scans that often lacked exactness and quality, today the imaging community has highly enhanced CT capabilities as well as MRI, PET/CT and SPECT/CT imaging. Better image quality enables greater accuracy in patient positioning, targeting the tumor as well as tracking the lesion during treatment. This minute localization offers customization and safety at unparalleled levels.
The right indications for SBRT
While SBRT represents a significant advancement in radiation therapy, determining the best methods and indications for use is currently a matter for careful analysis.
“We view SBRT as a very important emerging technology in the spectrum of cancer care, but feel it should first be performed in a very controlled and systematic fashion under clinical trials,” said Timothy D. Solberg, Ph.D., FACMP, FAAPM, professor and director, department of radiation oncology, University of Texas Southwestern Medical Center. “There’s significant promise from this technology, and preliminary studies are showing it as an effective and safe treatment. But there is potential for adverse effects if used improperly, and there is much to learn about its ideal use.”
From a technical point of view, the aspects of SBRT that are so exciting are also the most challenging. The confluence of imaging, positioning, tumor motion and high radiation presents much room for error and much to research. As the technology is so new, the field lacks critical information on dose fraction schemes that will optimize tumor control while maintaining morbidity at acceptable levels. Rigorous institutional study can address both the technological and clinical challenges inherent in SBRT, and determine the best specialized training for physicists, physicians and technicians.
“It’s not rational for every hospital in a major metropolitan area to do liver transplants, for example,” said Solberg. “But with new radiotherapy technologies, centers can feel pressured into adopting new procedures, to jump on board as soon as possible to remain competitive and financially secure. The radiation oncology community must approach new modalities like SBRT slowly and rationally. Use of SBRT should start in centers of excellence who do the initial work and train future practitioners.”
With research and establishment of best practices in SBRT in process, including several studies at Solberg’s facility, areas of possible use for the system are adding up. Oncologists are eying SBRT as a potential boon for tumors, metastases, sarcomas and more in areas like the spine, lung, pancreas, liver, prostate and the musculoskeletal system.
SBRT tools
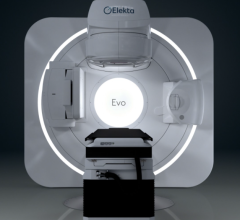
SBRT technology is so far led by a partnership between two key companies, Varian Medical Systems, a manufacturer of oncological radiotherapy options, and BrainLAB, a producer of medical technology and image-guided systems. The result of the partnership is the NovalisTX.
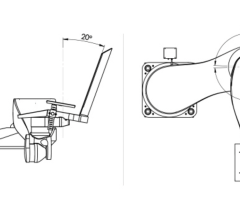
The NovalisTX’s beams are designed for delivering doses over 60 percent faster than conventional tools. Radiation delivery is guided by an advanced set of imaging options, including stereo X-ray 6D targeting, cone-beam CT and fluoroscopy. Proper patient positioning is achieved through adaptive gating and a robotic couch correction. Radiation is delivered through a high-definition multileaf collimator to shape treatment to specific tumors and placement. The NovalisTX promises flexibility, enhanced functionality, improved patient care and increased numbers of treated patients.
“In terms of our technological platform, Novalis offers no compromises,” said Huntzinger. The array of tools the system offers a medical team includes localization, treatment planning and dose sculpting.
SBRT may also impart economic benefits, as fewer treatment sessions, more effective and less damaging dose delivery and faster patient recovery translate into decreased overall cost.
With careful study and testing, and the advent of highly advanced tools like the NovalisTX, the future looks bright for SBRT.
“In the short term, caution with SBRT is key, and use should start with specialized centers, with rigorous programs for training new practitioners," said Solberg. "SBRT represents a profound paradigm shift for radiation oncology, with broader implications over the entire healthcare continuum, so in the long term, there will be widespread adoption of SBRT throughout the oncology community.”


 June 14, 2024
June 14, 2024