Breast biopsy rates grew quite dramatically during the latter part of the 20th century, and radiologists performed the majority of those procedures, according to a new Medicare database analysis. But as has been the case of late, radiologists did have to contend with some competition in this arena. “I think anybody who does breast imaging is well aware that there is a conflict – at many institutions, many departments, many practice groups – between radiologists and surgeons over who should be doing breast biopsies,” said David Levin, M.D., during a presentation at the 2005 RSNA meeting in Chicago. “The goal of this particular study was to determine which specialties perform the most breast biopsy and to examine recent trends in the practice patterns of these procedures.” Dr. Levin’s group at Thomas Jefferson University in Philadelphia used data from the U.S. Centers for Medicare and Medicaid Services (CMS) Physician/Supplier Procedure Summary Master Files for the years 1999 to 2003. The database provided exam volume and provider specialty for each of the Current Procedural Terminology (CPT) codes assigned to breast biopsy. “We studied the four surgical codes for breast biopsy of any type,” Dr. Levin explained. “We did not count the supervision and interpretation codes because that would lead to duplication of procedure numbers. We used specialty codes to classify providers as radiologists, surgeons (breast, general), and then all other physicians.” The following are the main CPT codes for breast biopsy used for this study: • 19100 – Biopsy of the breast (percutaneous, needle, core) without imaging guidance • 19101 – Biopsy of the breast (open, surgical) without imaging guidance • 19102 – Biopsy of the breast (percutaneous, needle, core) with imaging guidance • 19103 – Biopsy of the breast (percutaneous, automated, vacuum-assisted) with imaging guidance Dr. Levin said that his group did not include the CPT code for surgical excision of lesions as that was outside the scope of this biopsy-specific study. The authors first extracted the total utilization rate of breast biopsy per 1,000 Medicare fee-for-service beneficiaries. In 1999, the utilization rate was 265 per 1,000. In 2003, the figure jumped by 35 percent. They also determined that 83 percent of all breast biopsies were done with imaging. Based on physician specialty, 62 percent of all breast biopsies were performed by radiologists, while surgeons did 33 percent of the procedures. Other physicians handled five percent. “Radiologists clearly dominated,” Levin said. “If we look just at the two codes that used imaging, radiologists do 72 percent of all breast biopsies that utilize imaging for guidance. Surgeons do only 24 percent. Other physicians do about four percent.” Finally, the group extracted overall trends in breast biopsy. Dr. Levin pointed out that in 1999 radiologists did perform more biopsies, but not much more than surgeons. However, by 2003, “there [was] a very healthy upswing in the number of procedures performed by radiologists. The surgical trend line remained relatively flat,” he said. From 1999 to 2003, the total volume increase in breast biopsy procedures was 50 percent, with an 84 percent increase among radiologists versus 25 percent among surgeons. “The conclusions of our study are that within the Medicare population – and I don't really see why this should be any different in the commercial population – the rate at which breast biopsy is being performed is increasing,” Dr. Levin said. “Secondly, most breast biopsies are being done with imaging guidance. Third, radiologists perform the majority of breast biopsies.” In response to a question from an RSNA attendee, Dr. Levin said his group could not calculate how many surgical biopsies were preceded by wire localization. That kind of information was not available in this CMS database, Dr. Levin explained, and would have required access to individual patient records. Another audience member suggested that all of radiology could learn a lesson from breast imagers by making more of an effort to reach out to patients and possibly prevent other specialists from horning in on their territory. “It’s easy to grouse about self-referral," he commented. "One of the unique features of mammographers is that they tend to interact with patients as real, live human beings. I think the numbers make a case that we can be real clinicians and we can compete in the arena of self-referral.” Shalmali Pal is a staff writer with AuntMinnie.com. This story was reprinted with permission of AuntMinnie.com
If you enjoy this content, please share it with a colleague
Related Content
September 14, 2023 — Insight Medbotics, a medical device company combining the accuracy of MRI with the precision of ...
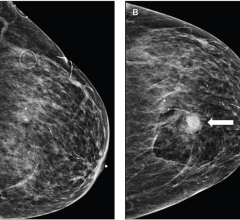
May 11, 2023 — According to an accepted manuscript published in ARRS’ own American Journal of Roentgenology (AJR) ...
September 9, 2022 — According to ARRS’ American Journal of Roentgenology (AJR), ultrasound color Doppler twinkling may ...
March 4, 2022 — The WTA and Hologic today jointly announced a landmark partnership introducing Hologic as the global ...
July 7, 2021 — GE Healthcare announced the installation of Serena Bright in five hospitals and radiology centers around ...
October 26, 2020 — iCAD, Inc. announced the Company will showcase the expanded platform for the Xoft Axxent Electronic ...
September 8, 2020 — Advanced Radiation Therapy has completed the installation of the AccuBoost Digital platform at the ...
August 28, 2020 — Hologic, Inc., an innovative medical technology company primarily focused on improving women’s health ...
November 26, 2019 — Unifi Workspace, a new comprehensive breast diagnostic reading solution from Hologic, will launch at ...
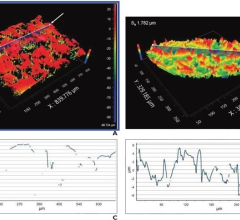
The current body of research supporting digital breast tomosynthesis (DBT or 3-D mammography) is now overwhelming, with ...


 September 14, 2023
September 14, 2023