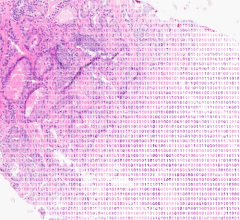
Advances in molecular imaging, specifically through the discovery of new molecular imaging agents and developments in the technologies that enable their visualization have opened up new possibilities for the early detection of disease as well as personalized medicine.
In conventional radioimmunoimaging (RAII), radioisotopes are bound with therapeutic antibodies and are administered concurrently to targets of disease. Delivering both the imaging and therapeutic agents together lowers the sensitivity and the selectivity of the radioimmunoimaging due to the antibody taking more time to leave the body, resulting in less accurate images and less lethal doses of radiation to the tumor. In contrast, pretargeting yields more precise images due to a high signal with very low background noise and a more toxic radioactive dose to the tumor while sparing healthy tissue.
More predictable treatments
The breakthrough technique, pretargeting, shows much hope for the effective and early treatment of cancer. Otto Boerman, Ph.D., professor in the department of nuclear medicine at Radbound University Nijmegen Medical Center, Nijmegen, The Netherlands, led a study examining the potential of pretargeting which was recently presented at the Society of Nuclear Medicine’s 55th Annual Meeting.
Pretargeting “decouple(s) the delivery of the bispecific antibody that seeks out the disease-carrying cells from the delivery of the imaging or therapeutic radioisotope. During the few-day-waiting period between the delivery of the bispecific antibody and the delivery of the radioisotope, the unbound antibody clears from the body, leaving only the tumor-bound antibody behind. This ensures that the radioisotope binds only to the tumor cells and not to the other bystander tissues in the body, thus improving the tumor-to-nontumor ratio of the radioisotope greater than 100-fold compared to the directly labeled antibodies,” according to Boerman.
According to Boerman, in this process a bispecific monoclonal antibody (bsMAb), with one arm that recognizes a tumor-associated antigen and another arm that recognizes a peptide carrying an imaging agent, is given as a first injection. When the non-tumor-bound bsMAb has substantially cleared non-target tissues and has reached a maximum level in the tumor, the bsMAb-recognizable imaging agent is given. The latter agent either targets the bsMAb localized at the tumor or is rapidly removed in the urine. Because the delivery of imaging isotopes is rapid and is separated from the long antibody delivery process, radioisotope uptake in the tumor is significantly higher than in the blood, making pretargeting RAII an attractive alternative to traditional RAII.
“Because the same bispecific antibody can be used with both imaging and therapeutic isotopes, this approach lends itself to use in personalized medicine, where the sequence of steps would be as follows — delivery of the bispecific antibody, delivery of an imaging isotope, imaging to confirm targeting of the tumor by the antibody and delivery of the therapeutic isotope. In this sequence, the imaging step serves as a predictive tool for the success of the therapeutic step, making the approach highly attractive to patients, physicians and managed care organizations,” Boerman explained.
Traditional monoclonal antibody treatments cost over $20,000 per treatment cycle but achieve results in less than 50 percent of cases. Because of the inability of this technique to appropriately target disease, pretargeting offers a way to predict whether a certain antibody will appropriately target the cancer.
Several new pretargeting agents for cancer have been developed, according to Boerman, including an anti-CEA agent that attaches to colorectal, breast and lung cancers; an anti-CD20 agent that attaches to leukemia and lymphoma cells; and an anti-MUC1 agent that very specifically attaches to the pancreatic cancer cells. These pretargeting agents can be used with any type of imaging tool such as PET, ultrasound, MRI and fluorescence.
Clearer vision of angiogenesis
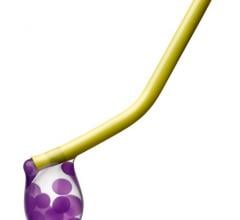
Other molecular imaging advances have been underway at GE Healthcare where researchers are using molecular agents to visualize angiogenesis, the formation of new blood vessels created by cancer — a product GE is calling “f-angio.”
Since cancer cells have the ability to form new blood vessels, particularly the more aggressive types of cancer, targeting the formation of new blood vessels would reveal the metabolism and the propensity of growth of a tumor and be able to detect lesions that are extremely small. Jean Luc Vanderheyden, Ph.D., global molecular imaging leader for GE Healthcare explained that clinical trials are currently being conducted using “f-angio” and said, “I’m just reporting anecdotal results here, but the ability to see breast metastases that are very small, hardly defined by CT but can be seen by MI [molecular imaging] techniques, have been reported by researchers.”
Along with the discovery of these new molecular agents, new imaging tools have been created to enhance their visualization. The ultimate endpoint in this endeavor has been achieving motion-free image acquisition. Breathing itself or the heart beating is enough to blur images of small tumors, so a new approach is to separate the focus of the image from the background.
“If you are affecting things that are very small, it is important to have the equipment that is capable of separating these areas from the background and that is where technology has taken place; where we have developed MotionFree software, which is not just software but is a way to acquire the data and render it in 4D mode,” Vanderheyden explained.
The ability to track a tumor over time has implications in the area of radiation therapy where the motion of a tumor may hinder treatment if not taken into account in the treatment planning. Using the latest VUE Point HD high-definition imaging with crystal technology by GE Healthcare in combination with other MotionFree techniques helps improve lesion detectability, treatment planning and quantitative accuracy, improving contrast-to-noise of moving lesions up to 60 percent versus static acquisition for overall better clinical confidence.
Also enabling better visualization of molecular imaging agents is the Infinia Hawkeye 4 by GE Healthcare, which is a multislice helical SPECT/CT delivering higher image quality and fast patient throughput that delivers high- quality attenuation correction for every SPECT procedure and precise localization, thus improving diagnostic confidence as demonstrated by more than 70 peer-reviewed scientific publications.
Another PET/CT product by GE Healthcare that assists in evaluating the treatment efficacy of a patient is the PET VCAR (Volume Computer-Assisted Reading), which has the ability to quantify cancer disease from a volume of PET data. The PET VCAR enables easy exam-to-exam comparison for fast review, multiple segmentation algorithms to help define tumor volumes and a multi-planar or orthogonal image review tool for different visual anatomical perspectives. Vanderheyden commented, “The PET VCAR’s strength is in its ability to use the patient for its own control — meaning a patient would go in before a treatment and you can see what the metabolism is of the different tumors so that after they get their treatment whether it be chemo or another way, the patient goes back and gets another molecular imaging procedure that you can compare with the first…the volumetric aspect of the CT gives you the map in a morphology point of view so that you can superimpose and get an idea of whether the tumor is regressing, is it the same or is it increasing.”
These new imaging advances open the doors for a greater merger between imaging and therapy, allowing one to determine whether a certain therapy is appropriate and/or effective as it enables detecting disease at earlier stages. Looking toward the future, making referring physicians aware of the advances in the field of molecular imaging and cancer treatment is key because, according to Vanderheyden, there is evidence that patients are not being referred enough to some imaging procedures even though FDG glucose procedures are already being strongly reimbursed. In addition, clinical trials must continue to demonstrate the efficacy of these treatments. “At that point, I think there will be ample way and evidence to use molecular imaging much more broadly at a much more visible and earlier part of a patient’s journey; to be used in the future much more prospectively in finding diseases earlier and therefore also following up if the treatment is appropriate.”


 November 11, 2025
November 11, 2025